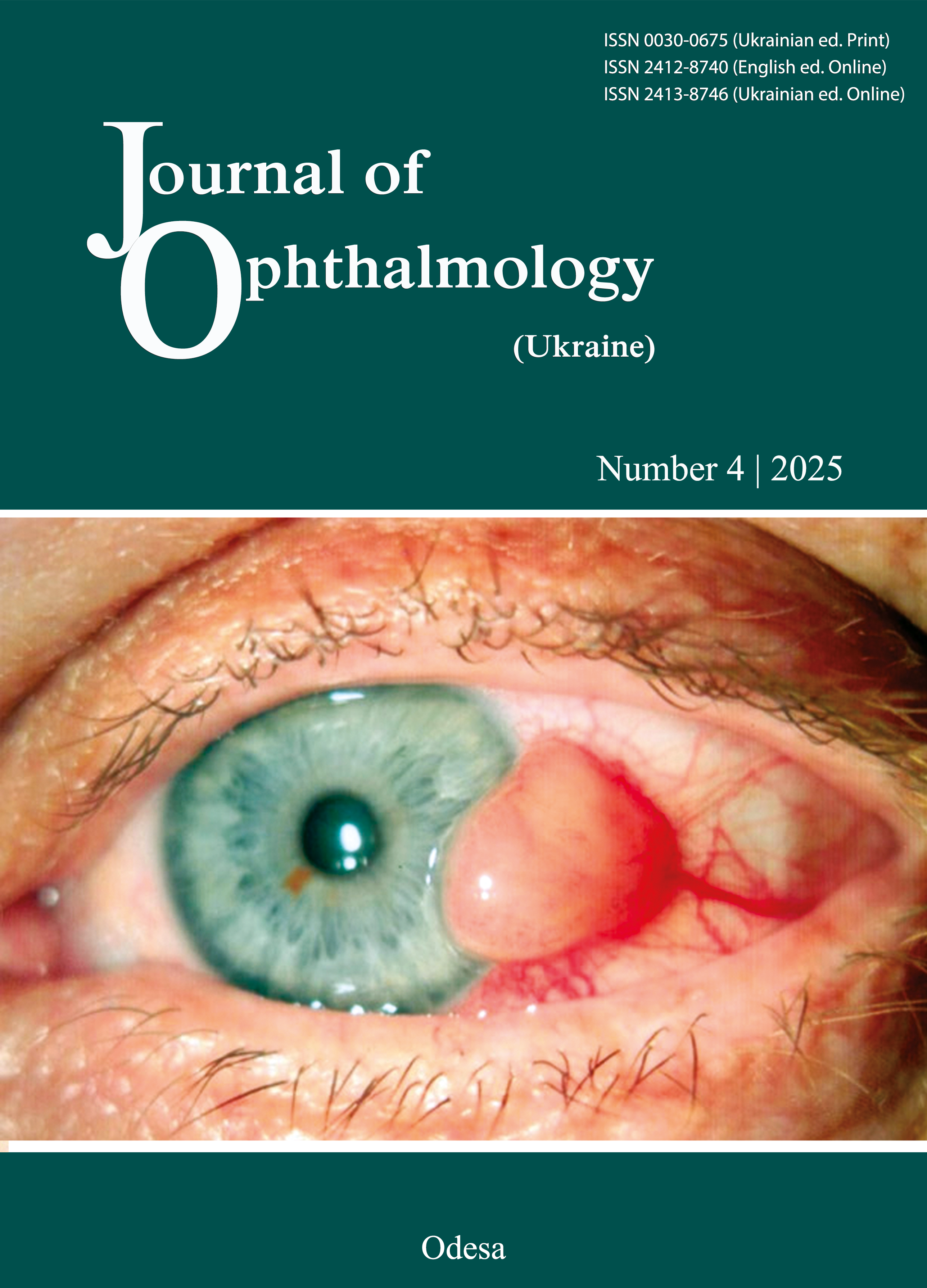
Prolonged Hospital Stay in Corneal Ulcer: Association with Sociodemographic and Clinical Factors
DOI:
https://doi.org/10.31288/oftalmolzh20254914Keywords:
cornea, corneal ulcer, hospitalization, microbial keratitis, fungal keratitis, prolonged hospital stay, predictors, diabetes, hypopyon, treatment delay, ocular infectionAbstract
Background. Corneal ulcers are a major cause of visual impairment and blindness, particularly in developing regions. While hospitalization is often necessary for severe cases, the factors influencing prolonged hospital stays remain inadequately explored. Identifying key sociodemographic and clinical predictors can aid in optimizing patient management and resource allocation.
Objective. This study aims to assess the sociodemographic and clinical factors associated with prolonged hospitalization in patients with corneal ulcers.
Methods. A retrospective observational study was conducted over one year with a sample size of 200 hospitalized patients diagnosed with corneal ulcers. Data were collected on sociodemographic variables (age, gender, socioeconomic status, rural vs. urban Residence) and clinical characteristics (ulcer size, depth, microbial aetiology, hypopyon presence, diabetes, immunosuppression, prior ocular surgery, treatment delay, and need for surgical Intervention). Length of hospital stay was categorized as prolonged vs. non-prolonged, and statistical analyses, including multivariate regression, were performed to identify independent predictors.
Results. Prolonged hospitalization was significantly associated with larger ulcer size (p < 0.01), fungal aetiology (p < 0.05), presence of hypopyon (p < 0.01), delayed treatment (p < 0.01), and diabetes mellitus (p < 0.05). Patients with fungal ulcers had higher complication rates and required extended inpatient care. Rural patients experienced delayed diagnosis and referral, contributing to longer hospital stays. Multivariate analysis confirmed that microbial aetiology, ulcer severity, and systemic comorbidities were independent predictors of prolonged hospitalization.
Conclusion. Early diagnosis and prompt treatment are critical in reducing hospitalization duration and improving outcomes in corneal ulcer patients. Strengthening primary eye care services, community-based screening, and outpatient follow-up can mitigate the burden of prolonged hospitalization. Further multicenter studies and prospective trials are warranted to validate these findings and explore innovative treatment approaches.
References
Akosman S, Li R, Kwon B, West W, Asahi M, Wroblewski KJ. Sociodemographic and clinical predictors of prolonged length of corneal ulcer hospitalizations. JAMA Ophthalmol. 2024;142(3):235-241. https://doi.org/10.1001/jamaophthalmol.2023.6512
Maretz C, Atlas J, Shah S, Sohn MB, Wozniak RA. Infectious keratitis in Western New York: a 10-year review of patient demographics, clinical management, and treatment failure. Front Ophthalmol. 2024;4:1469966. https://doi.org/10.3389/fopht.2024.1469966
Romero-Duarte Á, Rivera-Izquierdo M, Guerrero-Fernández de Alba I, Pérez-Contreras M, Fernández-Martínez NF, Ruiz-Montero R, et al. Sequelae, persistent symptomatology and outcomes after COVID-19 hospitalization: the ANCOHVID multicentre 6-month follow-up study. BMC Med. 2021;19:129. https://doi.org/10.1186/s12916-021-02003-7
Prajna NV, Radhakrishnan N, Sharma S. Prevention in the management of infectious keratitis. JAMA Ophthalmol. 2024;142(3):241-242. https://doi.org/10.1001/jamaophthalmol.2023.6784
Tze-Suen C, Chew-Ean T, Din NM. Fungal keratitis in a tertiary hospital in Malaysia. Cureus. 2021;13(9):e17975. doi:10.7759/cureus.17975 https://doi.org/10.7759/cureus.17975
Chow TS, Tan CE, Norshamsiah MD. Fungal keratitis in a tertiary hospital in Malaysia. Cureus. 2021;13(9):e17975. https://doi.org/10.7759/cureus.17975
Razi-Chafi Z, Esmaeilpour-Bandboni M, Salmalian Z. Prevalence of pressure ulcer and its related factors in elderly patients hospitalized to teaching hospitals in East Guilan. J CurrOncol Med Sci. 2023;3(1):375-381.
Ogoina D, Dalhat MM, Denue BA, Okowa M, Chika-Igwenyi NM, Yusuff HA, et al. Clinical characteristics and predictors of human mpox outcome during the 2022 outbreak in Nigeria: a cohort study. Lancet Infect Dis. 2023;23(12):1418-1428. https://doi.org/10.1016/S1473-3099(23)00427-9
Khoo P, Cabrera-Aguas MP, Nguyen V, Lahra MM, Watson SL. Microbial keratitis in Sydney, Australia: risk factors, patient outcomes, and seasonal variation. Graefes Arch ClinExpOphthalmol. 2020;258:1745-1755. https://doi.org/10.1007/s00417-020-04689-6
Sweeney C. Analyses of NSAID-Induced GI Bleed Related Hospitalization Discharges from 2016 to 2018 in the United States [dissertation]. Newark (NJ): Rutgers The State University of New Jersey, Rutgers School of Health Professions; 2022. Available from: https://rucore.libraries.rutgers.edu/rutgers-lib/67194/
Suárez-González P, Suárez-Elosegui A, Arias-Fernández L, Pérez-Regueiro I, Jimeno-Demuth FJ, Lana A. Nursing diagnoses and hospital readmission of patients with respiratory diseases: findings from a case-control study. Nurs Open. 2024;11(5):e2182. https://doi.org/10.1002/nop2.2182
Dweib M, El Sharif N. Diabetes-related microvascular complications in primary health care settings in the West Bank, Palestine. J Clin Med. 2023;12(21):6719. https://doi.org/10.3390/jcm12216719
Lee R, Manche EE. Trends and associations in hospitalizations due to corneal ulcers in the United States, 2002-2012. Ophthalmic Epidemiol. 2016;23(4):257-263. https://doi.org/10.3109/09286586.2016.1172648
Saeed A, D'Arcy F, Stack J, Collum LM, Power W, Beatty S. Risk factors, microbiological findings, and clinical outcomes in cases of microbial keratitis admitted to a tertiary referral center in Ireland. Cornea. 2009;28(3):285-292. https://doi.org/10.1097/ICO.0b013e3181877a52
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Indrajit Sarkar, Dattatreya Banerjee, Rashmirekha Behera

This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International (CC BY 4.0) that allows users to read, download, copy, distribute, print, search, or link to the full texts of the articles, or use them for any other lawful purpose, without asking prior permission from the publisher or the author as long as they cite the source.
COPYRIGHT NOTICE
Authors who publish in this journal agree to the following terms:
- Authors hold copyright immediately after publication of their works and retain publishing rights without any restrictions.
- The copyright commencement date complies the publication date of the issue, where the article is included in.
DEPOSIT POLICY
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) during the editorial process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work with an acknowledgement of its initial publication in this journal.
- Post-print (post-refereeing manuscript version) and publisher's PDF-version self-archiving is allowed.
- Archiving the pre-print (pre-refereeing manuscript version) not allowed.