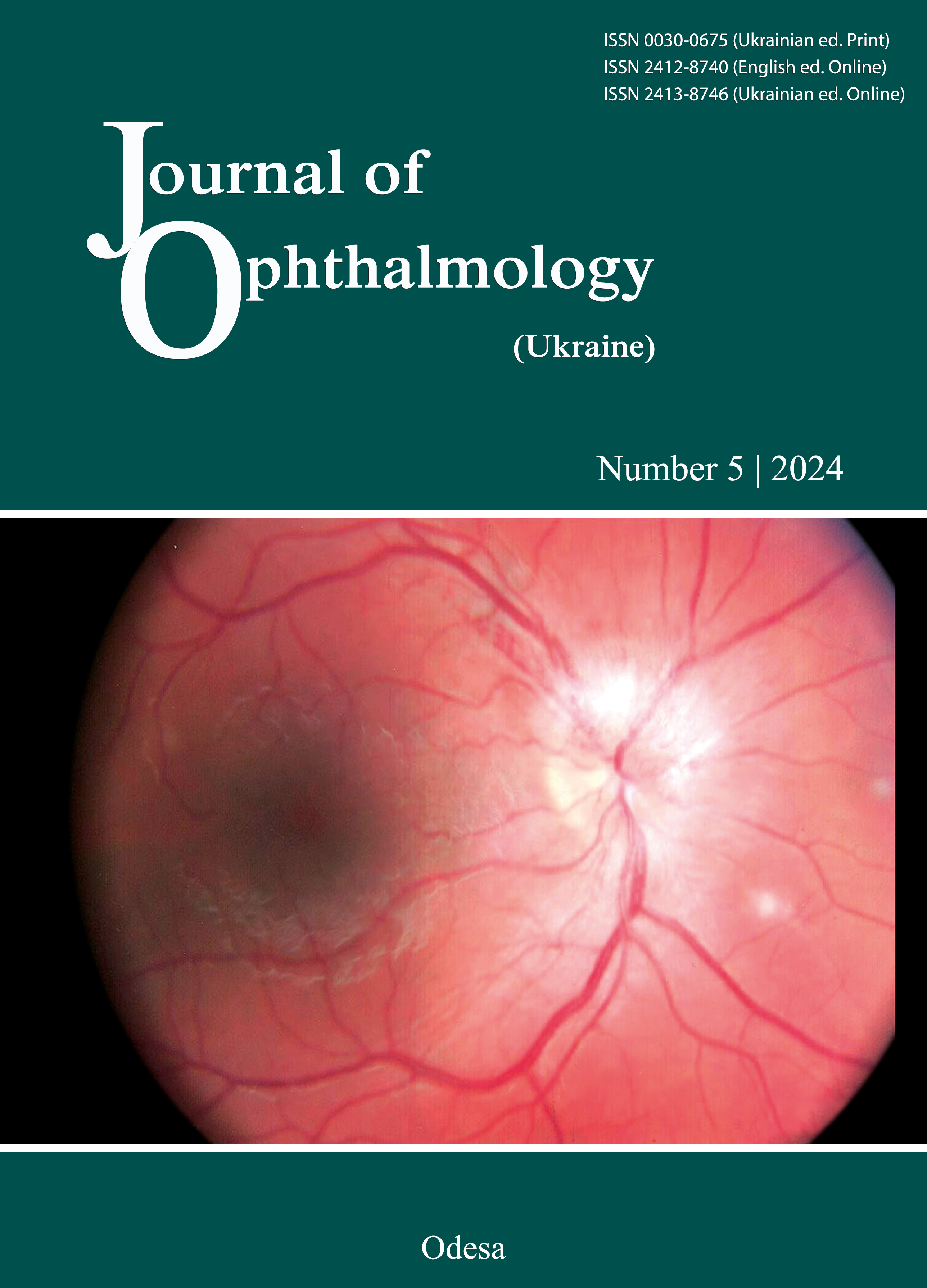
Uveitis Masquerade Syndrome
DOI:
https://doi.org/10.31288/oftalmolzh202453848Ключові слова:
Uveitis masquerade syndrome, Vitreoretinal lymphoma, Clinical registryАнотація
The ‘uveitis masquerade syndrome’ is a large group of neoplastic and non-neoplastic conditions that mimic and are initially misdiagnosed as uveitis. These eye diseases account for approximately 5% of all presentations at tertiary referral uveitis clinics. Vitreoretinal lymphoma is one of the most common of the neoplastic conditions that present as uveitis. With a 5-year survival rate under 50%, it is vitally important to recognize this diagnosis promptly. Other malignancies that may masquerade as uveitis include systemic lymphomas, primary uveal lymphoma, leukemias, multiple myeloma, uveal melanoma, metastatic cancers, and in children, retinoblastoma, medulloepithelioma, and post-transplantation lymphoproliferative disorder. Paraneoplastic syndromes are also possible uveitis mimics. Non-neoplastic conditions that may present as uveitis include the ocular ischemic syndrome and other vascular eye diseases, central serous chorioretinopathy, inherited retinal diseases, rhegmatogenous retinal detachment, pigment dispersion syndrome, intraocular foreign bodies, and in children, juvenile xanthogranuloma and Coats disease. In this article, we review the uveitis masquerade syndrome. Our major focus is vitreoretinal lymphoma, but we also summarize the other neoplasms and non-neoplastic diseases that may masquerade as uveitis.
Посилання
Rothova A, Groen F, Ten Berge J, et al. Causes and clinical manifestations of masquerade syndromes in intraocular inflammatory diseases. Retina. 2021;41(11):2318-24. https://doi.org/10.1097/IAE.0000000000003171
Hsu YR, Wang LU, Chen FT, et al. Clinical manifestations and implications of nonneoplastic uveitis masquerade syndrome. Am J Ophthalmol. 2022;238:75-85. https://doi.org/10.1016/j.ajo.2021.12.018
Grange LK, Kouchouk A, Dalal MD, et al. Neoplastic masquerade syndromes in patients with uveitis. Am J Ophthalmol. 2014;157(3):526-31. https://doi.org/10.1016/j.ajo.2013.11.002
Farrall AL, Smith JR. Eye involvement in primary central nervous system lymphoma. Surv Ophthalmol. 2020;65(5):548-61. https://doi.org/10.1016/j.survophthal.2020.02.001
Coupland SE, Heimann H, Bechrakis NE. Primary intraocular lymphoma: a review of the clinical, histopathological and molecular biological features. Graefes Arch Clin Exp Ophthalmol. 2004;242(11):901-13. https://doi.org/10.1007/s00417-004-0973-0
Sobolewska B, Chee SP, Zaguia F, et al. Vitreoretinal lymphoma. Cancers (Basel). 2021;13(16):3921. https://doi.org/10.3390/cancers13163921
Cimino L, Chan CC, Shen D, et al. Ocular involvement in nasal natural killer T-cell lymphoma. Int Ophthalmol. 2009;29(4):275-9. https://doi.org/10.1007/s10792-008-9220-8
Coupland SE, Anastassiou G, Bornfeld N, et al. Primary intraocular lymphoma of T-cell type: report of a case and review of the literature. Graefes Arch Clin Exp Ophthalmol. 2005;243(3):189-97. https://doi.org/10.1007/s00417-004-0890-2
Low A, Chow RC, Ee Ling A, Khaliddin N. Primary T-cell vitreoretinal non-hodgkin lymphoma: a case report and literature review. Cureus. 2023;15(7):e41341. https://doi.org/10.7759/cureus.41341
Alaggio R, Amador C, Anagnostopoulos I, et al. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Lymphoid Neoplasms. Leukemia. 2022;36(7):1720-48. https://doi.org/10.1038/s41375-022-01620-2
Riemersma SA, Jordanova ES, Schop RF, et al. Extensive genetic alterations of the HLA region, including homozygous deletions of HLA class II genes in B-cell lymphomas arising in immune-privileged sites. Blood. 2000;96(10):3569-77. https://doi.org/10.1182/blood.V96.10.3569
Farrall AL, Smith JR. Incidence and survival of ocular diffuse large B-cell lymphomas. Acta Ophthalmol. 2023;101(3):e353-4. https://doi.org/10.1111/aos.15284
Levasseur SD, Wittenberg LA, White VA. Vitreoretinal lymphoma: a 20-year review of incidence, clinical and cytologic features, treatment, and outcomes. JAMA Ophthalmol. 2013;131(1):50-5. https://doi.org/10.1001/jamaophthalmol.2013.569
Hong JT, Chae JB, Lee JY, et al. Ocular involvement in patients with primary CNS lymphoma. J Neurooncol. 2011;102(1):139-45. https://doi.org/10.1007/s11060-010-0303-9
Sjö LD. Ophthalmic lymphoma: epidemiology and pathogenesis. Acta Ophthalmol. 2009;87(thesis1):1-20. https://doi.org/10.1111/j.1755-3768.2008.01478.x
Haldorsen IS, Krossnes BK, Aarseth JH, et al. Increasing incidence and continued dismal outcome of primary central nervous system lymphoma in Norway 1989-2003: time trends in a 15-year national survey. Cancer. 2007;110(8):1803-14. https://doi.org/10.1002/cncr.22989
Corn BW, Marcus SM, Topham A, et al. Will primary central nervous system lymphoma be the most frequent brain tumor diagnosed in the year 2000? Cancer. 1997;79(12):2409-13. https://doi.org/10.1002/(SICI)1097-0142(19970615)79:12<2409::AID-CNCR17>3.0.CO;2-V
Jones NP, Pockar S, Steeples LR. Changing trends in uveitis in the United Kingdom: 5000 consecutive referrals to a tertiary referral centre. Ocul Immunol Inflamm. 2023;31(5):921-6. https://doi.org/10.1080/09273948.2022.2067067
Farrall AL, Smith JR. Changing incidence and survival of primary central nervous system lymphoma in Australia: a 33-year national population-based study. Cancers (Basel). 2021;13(3):403. https://doi.org/10.3390/cancers13030403
Menean M, Giuffrè C, Cicinelli MV, et al. A comprehensive overview of diagnosis, imaging and treatment of vitreoretinal lymphoma. Eur J Ophthalmol (in press).
von Roemeling C, Ferreri AJM, Soussain C, et al. Targets and treatments in primary CNS lymphoma. Leuk Lymphoma (in press).
Steffen J, Coupland SE, Smith JR. Primary vitreoretinal lymphoma in HIV infection. Ocul Immunol Inflamm. 2021;29(3):621-7. https://doi.org/10.1080/09273948.2020.1751856
Hochberg FH, Miller DC. Primary central nervous system lymphoma. J Neurosurg. 1988;68(6):835-53. https://doi.org/10.3171/jns.1988.68.6.0835
Ferreira LB, Furtado JM, Charng J, et al. Prevalence of toxoplasmic retinochoroiditis in an Australian adult population: a community-based study. Ophthalmol Retina. 2022;6(10):963-8. https://doi.org/10.1016/j.oret.2022.04.022
Shiels MS, Pfeiffer RM, Besson C, et al. Trends in primary central nervous system lymphoma incidence and survival in the U.S. Br J Haematol. 2016;174(3):417-24. https://doi.org/10.1111/bjh.14073
Motomura Y, Yoshifuji K, Tachibana T, et al. Clinical factors for central nervous system progression and survival in primary vitreoretinal lymphoma. Br J Haematol. 2024;204(4):1279-87. https://doi.org/10.1111/bjh.19266
Guan WX, Peng XY. Vitreoretinal lymphoma with intraretinal infiltration, simulating retinal necrosis. Ophthalmol Retina. 2024;8(6):571-8. https://doi.org/10.1016/j.oret.2023.11.016
Chan CC, Rubenstein JL, Coupland SE, et al. Primary vitreoretinal lymphoma: a report from an International Primary Central Nervous System Lymphoma Collaborative Group symposium. Oncologist. 2011;16(11):1589-99. https://doi.org/10.1634/theoncologist.2011-0210
Pichi F, Dolz-Marco R, Francis JH, et al. Advanced OCT analysis of biopsy-proven vitreoretinal lymphoma. Am J Ophthalmol. 2022;238:16-26. https://doi.org/10.1016/j.ajo.2021.11.023
Chiu S, Mudhar HS, Harrison B, et al. Cystoid macular oedema as a presenting feature of vitreoretinal lymphoma. Ocul Oncol Pathol. 2020;6(5):318-22. https://doi.org/10.1159/000508890
Hernández RF, Rodriguez JEM, Trecu MS, Bhatti MT. Not everything is ischemic optic neuropathy. Surv Ophthalmol (in press).
Zamani G, Hajipour A, Ganjeifar B, et al. Intraocular lymphoma masquerading as unilateral hypopyon anterior uveitis: a case report. J Ophthalmic Inflamm Infect. 2022;12(1):25. https://doi.org/10.1186/s12348-022-00302-5
Kvopka M, Lake SR, Smith JR. Intraocular chemotherapy for vitreoretinal lymphoma: a review. Clin Exp Ophthalmol. 2020;48(2):240-8. https://doi.org/10.1111/ceo.13668
Sehgal A, Pulido JS, Mashayekhi A, et al. Diagnosing vitreoretinal lymphomas - an analysis of the sensitivity of existing tools. Cancers (Basel). 2022;14(3):598. https://doi.org/10.3390/cancers14030598
Pulido JS, Johnston PB, Nowakowski GS, et al. The diagnosis and treatment of primary vitreoretinal lymphoma: a review. Int J Retina Vitreous. 2018;4:18. https://doi.org/10.1186/s40942-018-0120-4
Barajas RF, Politi LS, Anzalone N, et al. Consensus recommendations for MRI and PET imaging of primary central nervous system lymphoma: guideline statement from the International Primary CNS Lymphoma Collaborative Group (IPCG). Neuro Oncol. 2021;23(7):1056-71. https://doi.org/10.1093/neuonc/noab020
Carbonell D, Mahajan S, Chee S-P, et al. Consensus recommendations for the diagnosis of vitreoretinal lymphoma. Ocul Immunol Inflamm. 2021;29(3):507-20. https://doi.org/10.1080/09273948.2021.1878233
Yang X, Dalvin LA, Mazloumi M, et al. Spectral domain optical coherence tomography features of vitreoretinal lymphoma in 55 eyes. Retina. 2021;41(2):249-58. https://doi.org/10.1097/IAE.0000000000002819
Guan W, Xiao Y, Zhao H, et al. Spectral-domain optical coherence tomography biomarkers in vitreoretinal lymphoma. Clin Exp Ophthalmol. 2023;51(2):144-53. https://doi.org/10.1111/ceo.14197
Sen HN, Bodaghi B, Hoang PL, Nussenblatt R. Primary intraocular lymphoma: diagnosis and differential diagnosis. Ocul Immunol Inflamm. 2009;17(3):133-41. https://doi.org/10.1080/09273940903108544
Huang RS, Mihalache A, Popovic MM, et al. Diagnostic methods for primary vitreoretinal lymphoma: a systematic review. Surv Ophthalmol. 2024;69(3):456-64. https://doi.org/10.1016/j.survophthal.2023.12.001
Dawson AC, Williams KA, Appukuttan B, Smith JR. Emerging diagnostic tests for vitreoretinal lymphoma: a review. Clin Exp Ophthalmol. 2018;46(8):945-54. https://doi.org/10.1111/ceo.13304
Raja H, Salomão DR, Viswanatha DS, Pulido JS. Prevalence of MYD88 L265P mutation in histologically proven, diffuse large B-cell vitreoretinal lymphoma. Retina. 2016;36(3):624-8. https://doi.org/10.1097/IAE.0000000000000996
Lobo A, Okhravi N, Adamson P, et al. Protocol for the use of polymerase chain reaction in the detection of intraocular large B-cell lymphoma in ocular samples. J Mol Diagn. 2007;9(1):113-21. https://doi.org/10.2353/jmoldx.2007.050121
Sugita S, Takase H, Sugamoto Y, et al. Diagnosis of intraocular lymphoma by polymerase chain reaction analysis and cytokine profiling of the vitreous fluid. Jpn J Ophthalmol. 2009;53(3):209-14. https://doi.org/10.1007/s10384-009-0662-y
Wang Y, Shen D, Wang VM, et al. Molecular biomarkers for the diagnosis of primary vitreoretinal lymphoma. Int J Mol Sci. 2011;12(9):5684-97. https://doi.org/10.3390/ijms12095684
Frenkel S, Pe'er J, Kaufman R, et al. The importance of cytokines analysis in the diagnosis of vitreoretinal lymphoma. Acta Ophthalmol. 2020;98(6):e668-73. https://doi.org/10.1111/aos.14347
Bonzheim I, Giese S, Deuter C, et al. High frequency of MYD88 mutations in vitreoretinal B-cell lymphoma: a valuable tool to improve diagnostic yield of vitreous aspirates. Blood. 2015;126(1):76-9. https://doi.org/10.1182/blood-2015-01-620518
Giuffrè C, Cicinelli MV, Marchese A, et al. Clinical experience in a large cohort of patients with vitreoretinal lymphoma in a single center. Ocul Immunol Inflamm. 2021;29(3):472-8. https://doi.org/10.1080/09273948.2020.1787460
Demirci H, Rao RC, Elner VM, et al. Aqueous humor-derived MYD88 L265P mutation analysis in vitreoretinal lymphoma: a potential less invasive method for diagnosis and treatment response assessment. Ophthalmol Retina. 2023;7(2):189-95. https://doi.org/10.1016/j.oret.2022.08.005
Costopoulos M, Touitou V, Golmard JL, et al. ISOLD: a new highly sensitive interleukin score for intraocular lymphoma diagnosis. Ophthalmology. 2016;123(7):1626-8. https://doi.org/10.1016/j.ophtha.2016.01.037
Kuo DE, Wei MM, Knickelbein JE, et al. Logistic regression classification of primary vitreoretinal lymphoma versus uveitis by interleukin 6 and interleukin 10 levels. Ophthalmology. 2020;127(7):956-62. https://doi.org/10.1016/j.ophtha.2020.01.042
Nguyen NV, Khan F, Cannon A, et al. Diagnosis of primary vitreoretinal lymphoma masquerading infectious retinitis by retinal biopsy. J Ophthalmic Inflamm Infect. 2024;14(1):8. https://doi.org/10.1186/s12348-024-00389-y
Mastropasqua R, Thaung C, Pavesio C, et al. The role of chorioretinal biopsy in the diagnosis of intraocular lymphoma. Am J Ophthalmol. 2015;160(6):1127-32.e1. https://doi.org/10.1016/j.ajo.2015.08.033
Riemens A, Bromberg J, Touitou V, et al. Treatment strategies in primary vitreoretinal lymphoma: a 17-center European collaborative study. JAMA Ophthalmol. 2015;133(2):191-7. https://doi.org/10.1001/jamaophthalmol.2014.4755
Castellino A, Pulido JS, Johnston PB, et al. Role of systemic high-dose methotrexate and combined approaches in the management of vitreoretinal lymphoma: a single center experience 1990-2018. Am J Hematol. 2019;94(3):291-8. https://doi.org/10.1002/ajh.25350
Gao J, Peng X, Wang L. Efficacy and safety of first-line combination therapy versus monotherapy for vitreoretinal lymphoma: a systematic review and meta-analysis. BMC Ophthalmol. 2023;23(1):477. https://doi.org/10.1186/s12886-023-03226-3
Soussain C, Malaise D, Cassoux N. Primary vitreoretinal lymphoma: a diagnostic and management challenge. Blood. 2021;138(17):1519-34. https://doi.org/10.1182/blood.2020008235
Smith JR, Rosenbaum JT, Wilson DJ, et al. Role of intravitreal methotrexate in the management of primary central nervous system lymphoma with ocular involvement. Ophthalmology. 2002;109(9):1709-16. https://doi.org/10.1016/S0161-6420(02)01125-9
Habot-Wilner Z, Frenkel S, Pe'er J. Efficacy and safety of intravitreal methotrexate for vitreo-retinal lymphoma - 20 years of experience. Br J Haematol. 2021;194(1):92-100. https://doi.org/10.1111/bjh.17451
Sen HN, Chan CC, Byrnes G, et al. Intravitreal methotrexate resistance in a patient with primary intraocular lymphoma. Ocul Immunol Inflamm. 2008;16(1):29-33. https://doi.org/10.1080/09273940801899764
Larkin KL, Saboo US, Comer GM, et al. Use of intravitreal rituximab for treatment of vitreoretinal lymphoma. Br J Ophthalmol. 2014;98(1):99-103. https://doi.org/10.1136/bjophthalmol-2013-304043
Kakkassery V, Heindl LM, Rokohl AC, et al. Primary vitreoretinal lymphoma therapy monitoring: significant vitreous haze reduction after intravitreal rituximab. Neurosignals. 2021;29(S1):1-7. https://doi.org/10.33594/000000367
Dalvin LA, Lim LS, Ancona-Lezama D, et al. Tumor control and visual acuity outcomes in vitreoretinal lymphoma with and without sub-retinal pigment epithelium infiltration: analysis of 125 eyes of 70 patients at a single ocular oncology center. Ophthalmol Retina. 2019;3(11):998-1005. (doi:10.1016/j.oret.2019.05.021) https://doi.org/10.1016/j.oret.2019.05.021
Guneri Beser B, Demirci H. Intravitreal melphalan injection as a second-line local therapy in vitreoretinal lymphoma: case series. Retina. 2024;44(2):353-9. https://doi.org/10.1097/IAE.0000000000003963
Isobe K, Ejima Y, Tokumaru S, et al. Treatment of primary intraocular lymphoma with radiation therapy: a multi-institutional survey in Japan. Leuk Lymphoma. 2006;47(9):1800-5. https://doi.org/10.1080/10428190600632881
de la Fuente MI, Alderuccio JP, Reis IM, et al. Bilateral radiation therapy followed by methotrexate-based chemotherapy for primary vitreoretinal lymphoma. Am J Hematol. 2019;94(4):455-60. https://doi.org/10.1002/ajh.25414
Frigault MJ, Dietrich J, Gallagher K, et al. Safety and efficacy of tisagenlecleucel in primary CNS lymphoma: a phase 1/2 clinical trial. Blood. 2022;139(15):2306-15. https://doi.org/10.1182/blood.2021014738
PDQ® Adult Treatment Editorial Board. PDQ Primary CNS Lymphoma Treatment. Bethesda, MD: National Cancer Institute. Updated 02/12/2022. Available at: https://www.cancer.gov/types/lymphoma/hp/primary-cns-lymphoma-treatment-pdq. Accessed 19/07/2024.
Ahmed AH, Foster CS, Shields CL. Association of disease location and treatment with survival in diffuse large B-cell lymphoma of the eye and ocular adnexal region. JAMA Ophthalmol. 2017;135(10):1062-8. https://doi.org/10.1001/jamaophthalmol.2017.3286
Raval V, Binkley E, Aronow ME, et al. Primary central nervous system lymphoma - ocular variant: an interdisciplinary review on management. Surv Ophthalmol. 2021;66(6):1009-20. https://doi.org/10.1016/j.survophthal.2021.03.004
Rath A, Salamon V, Peixoto S, et al. A systematic literature review of evidence-based clinical practice for rare diseases: what are the perceived and real barriers for improving the evidence and how can they be overcome? Trials. 2017;18(1):556. https://doi.org/10.1186/s13063-017-2287-7
Fend F, Ferreri AJ, Coupland SE. How we diagnose and treat vitreoretinal lymphoma. Br J Haematol. 2016;173(5):680-92. https://doi.org/10.1111/bjh.14025
Smith JR, Farrall AL, Davis JL, et al. The International Vitreoretinal B-Cell Lymphoma Registry: a protocol paper. BMJ Open. 2022;12(7):e060701. https://doi.org/10.1136/bmjopen-2021-060701
The International Vitreoretinal B-Cell Lymphoma Registry Investigator Group. Presentation, diagnostic testing and initial treatment of vitreoretinal lymphoma. Ophthalmol Retina. 2024;8(1):72-80.
Farrall AL, Radford MHB, Smith JR. Comments on: Ophthalmic registries for rare eye diseases. Indian J Ophthalmol. 2023;71(3):1055-6. https://doi.org/10.4103/IJO.IJO_2606_22
Touhami S, Audo I, Terrada C, et al. Neoplasia and intraocular inflammation: from masquerade syndromes to immunotherapy-induced uveitis. Prog Retin Eye Res. 2019;72:100761. https://doi.org/10.1016/j.preteyeres.2019.05.002
Gaucher D, Bodaghi B, Charlotte F, et al. MALT-type B-cell lymphoma masquerading as scleritis or posterior uveitis. J Fr Ophtalmol. 2005;28(1):31-8. https://doi.org/10.1016/S0181-5512(05)81022-8
Sukon N, Tesavibul N, Choopong P, et al. Extranodal natural killer/T-cell lymphoma presenting as hypopyon panuveitis: a case report. BMC Ophthalmol. 2022;22(1):46. https://doi.org/10.1186/s12886-022-02277-2
Gauthier AC, Nguyen A, Munday WR, et al. Anterior chamber non-hodgkin lymphoma of the iris masquerading as uveitis-glaucoma-hyphema syndrome. Ocul Oncol Pathol. 2016;2(4):230-3. https://doi.org/10.1159/000445119
Moussa K, Begaj T, Ma K, et al. Systemic lymphoma masquerading as Vogt-Koyanagi-Harada syndrome: report of a case with multimodal imaging and histopathology. Am J Ophthalmol Case Rep. 2022;27:101643. https://doi.org/10.1016/j.ajoc.2022.101643
Mathai A, Lall A, Jain R, Pathengay A. Systemic non-Hodgkin's lymphoma masquerading as Vogt-Koyanagi-Harada disease in an HIV-positive patient. Clin Exp Ophthalmol. 2006;34(3):280-2. https://doi.org/10.1111/j.1442-9071.2006.01205.x
Panda P, Forooghian F, Goodglick T, et al. Orbital lymphoma masquerading as panuveitis. Ocul Immunol Inflamm. 2010;18(3):181-3. https://doi.org/10.3109/09273941003728947
Sonne SJ, Shieh WS, Srivastava SK, Smith BT. Lymphoma masquerading as occlusive retinal vasculitis: a case study. Am J Ophthalmol Case Rep. 2020;19:100777. https://doi.org/10.1016/j.ajoc.2020.100777
Rasić DM, Stanković Z, Terzić T, et al. Primary extranodal marginal zone lymphoma of the uvea associated with massive diffuse epibulbar extension and focal infiltration of the optic nerve and meninges, clinically presented as uveitis masquerade syndrome: a case report. Med Oncol. 2010;27(3):1010-6. https://doi.org/10.1007/s12032-009-9325-6
Wu RX, Yang T, Xu ZP. Primary uveal lymphoma effectively treated with radiotherapy: a case report and literature review. J South Med Univ. 2018;38(4):371-4.
Aronow ME, Portell CA, Sweetenham JW, Singh AD. Uveal lymphoma: clinical features, diagnostic studies, treatment selection, and outcomes. Ophthalmology. 2014;121(1):334-41. https://doi.org/10.1016/j.ophtha.2013.09.004
Vishnevskia-Dai V, Sella King S, Lekach R, et al. Ocular manifestations of leukemia and results of treatment with intravitreal methotrexate. Sci Rep. 2020;10(1):1994. https://doi.org/10.1038/s41598-020-58654-8
Hafeez MU, Ali MH, Najib N, et al. Ophthalmic manifestations of acute leukemia. Cureus. 2019;11(1):e3837. https://doi.org/10.7759/cureus.3837
Reddy SC, Jackson N, Menon BS. Ocular involvement in leukemia--a study of 288 cases. Ophthalmologica. 2003;217(6):441-5. https://doi.org/10.1159/000073077
Koshy J, John MJ, Thomas S, et al. Ophthalmic manifestations of acute and chronic leukemias presenting to a tertiary care center in India. Indian J Ophthalmol. 2015;63(8):659-64. https://doi.org/10.4103/0301-4738.169789
Guerriero S, Piscitelli D, Ciracì L, et al. Hypertensive uveitis as a feature of multiple myeloma. Ocul Immunol Inflamm. 2010;18(2):104-6. https://doi.org/10.3109/09273940903402645
Yew YC, Nurul-Fatin FS, Norazita AT. Multiple myeloma masquerading as panuveitis in a middle-aged woman. Med J Malaysia. 2017;72(6):376-7.
Singh RB, Singhal S, Sinha S, et al. Ocular complications of plasma cell dyscrasias. Eur J Ophthalmol. 2023;33(5):1786-800. https://doi.org/10.1177/11206721231155974
Buder K, Gesierich A, Gelbrich G, Goebeler M. Systemic treatment of metastatic uveal melanoma: review of literature and future perspectives. Cancer Med. 2013;2(5):674-86. https://doi.org/10.1002/cam4.133
Kafkala C, Daoud YJ, Paredes I, Foster CS. Masquerade scleritis. Ocul Immunol Inflamm. 2005;13(6):479-82. https://doi.org/10.1080/09273940591004133
Fraser DJ Jr, Font RL. Ocular inflammation and hemorrhage as initial manifestations of uveal malignant melanoma. Incidence and prognosis. Arch Ophthalmol. 1979;97(7):1311-4. https://doi.org/10.1001/archopht.1979.01020020053012
Abdel-Aty A, Linderman WL, Kombo N, et al. Necrotic uveal melanoma mimics orbital cellulitis: a review. Ocul Oncol Pathol. 2022;8(1):1-8. https://doi.org/10.1159/000515558
Berkowitz ST, Brock AL, Reichstein DA. An amelanotic choroidal melanoma arising in a young man with tattoo-associated sarcoidosis. Am J Ophthalmol Case Rep. 2020;18:100655. https://doi.org/10.1016/j.ajoc.2020.100655
Welch RJ, Newman JH, Honig SE, et al. Choroidal amelanotic tumours: clinical differentiation of benign from malignant lesions in 5586 cases. Br J Ophthalmol. 2020;104(2):194-201. https://doi.org/10.1136/bjophthalmol-2018-313680
Kaliki S, Shields CL. Uveal melanoma: relatively rare but deadly cancer. Eye. 2017;31(2):241-57. https://doi.org/10.1038/eye.2016.275
Shields CL, Shields JA, Gross NE, et al. Survey of 520 eyes with uveal metastases. Ophthalmology. 1997;104(8):1265-76. https://doi.org/10.1016/S0161-6420(97)30148-1
Nguyen QL, Reynolds SB, Piri N, Rivas Perez HL. Ophthalmic anterior segment metastasis masquerading as uveitis. BMJ Case Rep. 2021;14(3):e236405. https://doi.org/10.1136/bcr-2020-236405
Shields CL, McMahon JF, Atalay HT, et al. Retinal metastasis from systemic cancer in 8 cases. JAMA Ophthalmol. 2014;132(11):1303-8. https://doi.org/10.1001/jamaophthalmol.2014.2406
Shields CL, Welch RJ, Malik K, et al. Uveal metastasis: clinical features and survival outcome of 2214 tumors in 1111 patients based on primary tumor origin. Middle East Afr J Ophthalmol. 2018;25(2):81-90. https://doi.org/10.4103/meajo.MEAJO_6_18
Liu W, Ma W, Guo R, Ji J. Snowflakes in the eye - an uncommon presentation of iris metastasis of esophageal carcinoma and review of literature. Ocul Immunol Inflamm. 2022;30(7-8):1568-71. https://doi.org/10.1080/09273948.2021.1906910
Soheilian M, Mirbabai F, Shahsavari M, et al. Metastatic cutaneous melanoma to the vitreous cavity masquerading as intermediate uveitis. Eur J Ophthalmol. 2002;12(4):324-7. https://doi.org/10.1177/112067210201200413
Ozawa H, Usui Y, Takano Y, et al. Iris metastasis as the initial presentation of metastatic esophageal cancer diagnosed by fine needle aspiration biopsy: a case report. Medicine. 2021;100(22):e26232. https://doi.org/10.1097/MD.0000000000026232
Shields JA, Shields CL, Singh AD. Metastatic neoplasms in the optic disc: the 1999 Bjerrum Lecture: part 2. Arch Ophthalmol. 2000;118(2):217-24. https://doi.org/10.1001/archopht.118.2.217
Bhatnagar R, Vine AK. Diffuse infiltrating retinoblastoma. Ophthalmology. 1991;98(11):1657-61. https://doi.org/10.1016/S0161-6420(91)32072-4
Girard B, Le Hoang P, D'Hermies F, et al. Diffuse infiltrating retinoblastoma. J Fr Ophtalmol. 1989;12(5):369-81.
Shields CL, Ghassemi F, Tuncer S, et al. Clinical spectrum of diffuse infiltrating retinoblastoma in 34 consecutive eyes. Ophthalmology. 2008;115(12):2253-8. https://doi.org/10.1016/j.ophtha.2008.07.003
Domínguez-Varela IA, Aguilera-Partida JA, Dalvin LA, et al. Retinoblastoma in an older Hispanic child masquerading as pars planitis: a case report. Eur J Ophthalmol. 2022;32(3):NP71-4. https://doi.org/10.1177/1120672121994487
Panigrahi A, Singh A, Gupta S, Gupta V. Diffuse infiltrating retinoblastoma: a panuveitis masquerade. Can J Ophthalmol. 2023;58(6):e246-7. https://doi.org/10.1016/j.jcjo.2023.07.007
Traine PG, Schedler KJ, Rodrigues EB. Clinical presentation and genetic paradigm of diffuse infiltrating retinoblastoma: a review. Ocul Oncol Pathol. 2016;2(3):128-32. https://doi.org/10.1159/000441528
Font RL, Rishi K. Diffuse retinal involvement in malignant nonteratoid medulloepithelioma of ciliary body in an adult. Arch Ophthalmol. 2005;123(8):1136-8. https://doi.org/10.1001/archopht.123.8.1136
Shields JA, Eagle RC Jr, Shields CL, Potter PD. Congenital neoplasms of the nonpigmented ciliary epithelium (medulloepithelioma). Ophthalmology. 1996;103(12):1998-2006. https://doi.org/10.1016/S0161-6420(96)30394-1
Kanavi MR, Soheilian M, Kamrava K, Peyman GA. Medulloepithelioma masquerading as chronic anterior granulomatous uveitis. Can J Ophthalmol. 2007;42(3):474-6. https://doi.org/10.3129/i07-077
Chua J, Muen WJ, Reddy A, Brookes J. The masquerades of a childhood ciliary body medulloepithelioma: a case of chronic uveitis, cataract, and secondary glaucoma. Case Rep Ophthalmol Med. 2012;2012:493493. https://doi.org/10.1155/2012/493493
Tadepalli SH, Shields CL, Shields JA, Honavar SG. Intraocular medulloepithelioma - a review of clinical features, DICER 1 mutation, and management. Indian J Ophthalmol. 2019;67(6):755-62. https://doi.org/10.4103/ijo.IJO_845_19
Cook T, Grostern RJ, Barney NP, et al. Posttransplantation lymphoproliferative disorder initially seen as iris mass and uveitis. Arch Ophthalmol. 2001;119(5):768-70. https://doi.org/10.1001/archopht.119.5.768
Rohrbach JM, Kröber SM, Teufel T, et al. EBV-induced polymorphic lymphoproliferative disorder of the iris after heart transplantation. Graefes Arch Clin Exp Ophthalmol. 2004;242(1):44-50. https://doi.org/10.1007/s00417-003-0751-4
Cho AS, Holland GN, Glasgow BJ, et al. Ocular involvement in patients with posttransplant lymphoproliferative disorder. Arch Ophthalmol. 2001;119(2):183-9.
O'Hara M, Lloyd WC 3rd, Scribbick FW, Gulley ML. Latent intracellular Epstein-Barr Virus DNA demonstrated in ocular posttransplant lymphoproliferative disorder mimicking granulomatous uveitis with iris nodules in a child. J AAPOS. 2001;5(1):62-3. https://doi.org/10.1067/mpa.2001.112444
Iu LP, Yeung JC, Loong F, Chiang AK. Successful treatment of intraocular post-transplant lymphoproliferative disorder with intravenous rituximab. Pediatr Blood Cancer. 2015;62(1):169-72. https://doi.org/10.1002/pbc.25223
Przeździecka-Dołyk J, Brzecka A, Ejma M, et al. Ocular paraneoplastic syndromes. Biomedicines. 2020;8(11):490. https://doi.org/10.3390/biomedicines8110490
Sarkar P, Mehtani A, Gandhi HC, et al. Paraneoplastic ocular syndrome: a pandora's box of underlying malignancies. Eye (Lond). 2022;36(7):1355-67. https://doi.org/10.1038/s41433-021-01676-x
Shildkrot Y, Sobrin L, Gragoudas ES. Cancer-associated retinopathy: update on pathogenesis and therapy. Semin Ophthalmol. 2011;26(4-5):321-8. https://doi.org/10.3109/08820538.2011.588657
Terelak-Borys B, Skonieczna K, Grabska-Liberek I. Ocular ischemic syndrome - a systematic review. Med Sci Monit. 2012;18(8):RA138-44. https://doi.org/10.12659/MSM.883260
Hamed LM, Guy JR, Moster ML, Bosley T. Giant cell arteritis in the ocular ischemic syndrome. Am J Ophthalmol. 1992;113(6):702-5. https://doi.org/10.1016/S0002-9394(14)74798-1
Hayreh SS, Podhajsky PA, Zimmerman B. Ocular manifestations of giant cell arteritis. Am J Ophthalmol. 1998;125(4):509-20. https://doi.org/10.1016/S0002-9394(99)80192-5
Fukui A, Tanaka H, Terao N, et al. Changes in choroidal thickness and structure in preeclampsia with serous retinal detachment. J Clin Med. 2023;12(2):609. https://doi.org/10.3390/jcm12020609
Makhoul D, Kolyvras N, Benchekroun S, et al. Sickle cell crisis presenting as a masquerade syndrome complicated by macular ischemia. Ocul Immunol Inflamm. 2010;18(3):178-80. https://doi.org/10.3109/09273940903562232
Campagnoli TR, Krawitz BD, Lin J, et al. Salmon patch-associated vitreous hemorrhage in non-proliferative sickle cell retinopathy masquerading as infectious uveitis. Am J Ophthalmol Case Rep. 2022;25:101329. https://doi.org/10.1016/j.ajoc.2022.101329
Sharma A, Ibarra MS, Piltz-Seymour JR, Syed NA. An unusual case of uveitis-glaucoma-hyphema syndrome. Am J Ophthalmol. 2003;135(4):561-3. https://doi.org/10.1016/S0002-9394(02)02054-8
Lee DY, Chen SC, Sheu SJ. Coats disease masquerading as acute posterior uveitis in a young adult. Kaohsiung J Med Sci. 2022;38(2):178-9. https://doi.org/10.1002/kjm2.12451
Brockmann C, Löwen J, Schönfeld S, et al. Vascular findings in primarily affected and fellow eyes of middle-aged patients with Coats' disease using multimodal imaging. Br J Ophthalmol. 2021;105(10):1444. https://doi.org/10.1136/bjophthalmol-2020-317101
Chen PP, Chong LP. Coats'-like response in a patient with pars planitis. Br J Ophthalmol. 1996;80(7):675-6. https://doi.org/10.1136/bjo.80.7.675
Suh DW, Pulido JS, Jampol LM, et al. Coats'-like response in pars planitis. Retina. 1999;19(1):79-80. https://doi.org/10.1097/00006982-199901000-00015
Verma S, Bhatia I, Banerjee M, Kumar V. Coats like response in healed choroiditis. Ocul Immunol Inflamm. 2022;30(6):1527-9. https://doi.org/10.1080/09273948.2021.1887281
Pauleikhoff LJB, Diederen RMH, Chang-Wolf JM, et al. Choroidal hyperpermeability patterns correlate with disease severity in central serous chorioretinopathy: CERTAIN study report 2. Acta Ophthalmol (in press).
Tandon R, Vanathi M, Verma L, Bharadwaj A. Central serous retinopathy masquerading as sympathetic ophthalmia. Eye (Lond). 2003;17(5):666-7. https://doi.org/10.1038/sj.eye.6700423
Nagpal A, Biswas J. Pseudouveitis--analysis of cases misdiagnosed as posterior uveitis. Ocul Immunol Inflamm. 2006;14(1):13-20. https://doi.org/10.1080/09273940500545627
Liu Q, Hemarat K, Kayser DL, Stewart JM. A case of posterior uveal effusion syndrome masquerading as uveitis. Retin Cases Brief Rep. 2017;11(Suppl 1):S124-7. https://doi.org/10.1097/ICB.0000000000000463
Yoshida N, Ikeda Y, Notomi S, et al. Clinical evidence of sustained chronic inflammatory reaction in retinitis pigmentosa. Ophthalmology. 2013;120(1):100-5. https://doi.org/10.1016/j.ophtha.2012.07.006
Thenappan A, Nanda A, Lee CS, Lee SY. Retinitis pigmentosa masquerades: case series and review of the literature. J Clin Med. 2023;12(17):5620. https://doi.org/10.3390/jcm12175620
Mautone L, Birtel J, Atiskova Y, et al. X-linked retinoschisis masquerading uveitis. J Clin Med. 2023;12(11):3729. https://doi.org/10.3390/jcm12113729
Terrier B, Colombat M, Beugnet C, et al. Vitreous amyloidosis with autonomic neuropathy of the digestive tract associated with a novel transthyretin p.Gly87Arg variant in a Bangladeshi patient: a case report. J Med Case Rep. 2017;11(1):222. https://doi.org/10.1186/s13256-017-1407-z
Treviño-Herrera AB, Bustamante-Vargas AP, Lisker-Cervantes A, et al. Vitreous involvement as initial presentation of hereditary transthyretin amyloidosis related to the rare TTR Ile107Met (p.Ile127Met) pathogenic variant. Ophthalmic Genet. 2022;43(3):413-9. https://doi.org/10.1080/13816810.2022.2025606
O'Hearn TM, Fawzi A, He S, et al. Early onset vitreous amyloidosis in familial amyloidotic polyneuropathy with a transthyretin Glu54Gly mutation is associated with elevated vitreous VEGF. Br J Ophthalmol. 2007;91(12):1607-9. https://doi.org/10.1136/bjo.2007.119495
Lim WK, Chee SP. Retinal detachment in atopic dermatitis can masquerade as acute panuveitis with rapidly progressive cataract. Retina. 2004;24(6):953-6. https://doi.org/10.1097/00006982-200412000-00017
Joye AS, Bhisitkul RB, Pereira DDS, Gonzales JA. Rhegmatogenous retinal detachment masquerading as exudative panuveitis with intense anterior chamber inflammatory reaction. American J Ophthalmol Case Rep. 2020;18:100618. https://doi.org/10.1016/j.ajoc.2020.100618
Jarrett WH 2nd. Rhematogenous retinal detachment complicated by severe intraocular inflammation, hypotony, and choroidal detachment. Trans Am Ophthalmol Soc. 1981;79:664-83.
Uemura A.; Uto M. Bilateral retinal detachment with large breaks of pars plicata associated with coloboma lentis and ocular hypertension. Jpn J Ophthalmol. 1992;36(1):97-102.
Zeppieri M. Pigment dispersion syndrome: a brief overview. J Clin Transl Res. 2022;8(5):344-50.
Tugal-Tutkun I, Urgancioglu M. Bilateral acute depigmentation of the iris. Graefes Arch Clin Exp Ophthalmol. 2006;244(6):742-6. https://doi.org/10.1007/s00417-005-0137-x
Wefers Bettink-Remeijer M, Brouwers K, van Langenhove L, et al. Uveitis-like syndrome and iris transillumination after the use of oral moxifloxacin. Eye (Lond). 2009;23(12):2260-2. https://doi.org/10.1038/eye.2009.234
Gonul S, Bozkurt B. Bilateral acute iris transillumination (BAIT) initially misdiagnosed as acute iridocyclitis. Arq Bras Oftalmol. 2015;78(2):115-7. https://doi.org/10.5935/0004-2749.20150029
Niedzwiecka E, Cantó San Miguel MP, Gonzalez Herrera M, Sánchez Rodriguez-Acosta I. Bilateral acute depigmentation of the iris (BADI) following Covid-19 infection. Ocul Immunol Inflamm. 2023;31(6):1230-1. https://doi.org/10.1080/09273948.2022.2113801
Saifaoui N, Mnasri H, Dubiez M, El-Belhadji M. Case report: Intraocular foreign body masquerading as toxoplasma chorioretinitis. J Fr Ophtalmol. 2018;41(3):e113-5. https://doi.org/10.1016/j.jfo.2017.06.013
Politis M, Rosin B, Amer R. Ocular siderosis subsequent to a missed pars plana metallic foreign body that masqueraded as refractory intermediate uveitis. Ocul Immunol Inflamm. 2018;26(4):598-600.
Yeh S, Ralle M, Phan IT, et al. Occult intraocular foreign body masquerading as panuveitis: inductively coupled mass spectrometry and electrophysiologic analysis. J Ophthalmic Inflamm Infect. 2012;2(2):99-103. https://doi.org/10.1007/s12348-011-0035-9
Mahmoud A, Messaoud R, Abid F, et al. Anterior segment optical coherence tomography and retained vegetal intraocular foreign body masquerading as chronic anterior uveitis. J Ophthalmic Inflamm Infect. 2017;7(1):13. https://doi.org/10.1186/s12348-017-0130-7
Alexandrakis G, Balachander R, Chaudhry NA, Filatov V. An intraocular foreign body masquerading as idiopathic chronic iridocyclitis. Ophthalmic Surg Lasers. 1998;29(4):336-7. https://doi.org/10.3928/1542-8877-19980401-15
Kamath MG, Nayak IV, Satish KR. Case report: intraocular foreign body in the angle masquerading as uveitis. Indian J Ophthalmol. 1991;39(3):138-9.
Stangos AN, Pournaras CJ, Petropoulos IK. Occult anterior-chamber metallic fragment post-phacoemulsification masquerading as chronic recalcitrant postoperative inflammation. Am J Ophthalmol. 2005;139(3):541-2. https://doi.org/10.1016/j.ajo.2004.08.031
Wylegala E, Dobrowolski D, Nowińska A, Tarnawska D. Anterior segment optical coherence tomography in eye injuries. Graefes Arch Clin Exp Ophthalmol. 2009;247(4):451-5. https://doi.org/10.1007/s00417-008-0937-x
Cheng T, Zhao H, Chen Q, et al. Efficiency of different imaging methods in detecting ocular foreign bodies. Med Phys. 2024;51(4):3124-9. https://doi.org/10.1002/mp.16818
Esen Baris M, Ciftci MD, Palamar M, Guven Yilmaz S. Iris juvenile xanthogranuloma presenting with hypopyon. Ocul Immunol Inflamm. 2022;30(7-8):2014-6. https://doi.org/10.1080/09273948.2021.1936077
DeBarge LR, Chan CC, Greenberg SC, et al. Chorioretinal, iris, and ciliary body infiltration by juvenile xanthogranuloma masquerading as uveitis. Surv Ophthalmol. 1994;39(1):65-71. https://doi.org/10.1016/S0039-6257(05)80046-3
Zamir E, Wang RC, Krishnakumar S, et al. Juvenile xanthogranuloma masquerading as pediatric chronic uveitis: a clinicopathologic study. Surv Ophthalmol. 2001;46(2):164-71. https://doi.org/10.1016/S0039-6257(01)00253-3
Lahri B, Hussain Z, Gupta N, et al. Bilateral anterior uveitis as a presenting feature of juvenile xanthogranuloma in a neonate. Am J Ophthalmol Case Rep. 2023;31:101867. https://doi.org/10.1016/j.ajoc.2023.101867
Longmuir S, Dumitrescu A, Kwon Y, et al. Juvenile xanthogranulomatosis with bilateral and multifocal ocular lesions of the iris, cornealscleral limbus, and choroid. J AAPOS. 2011;15(6):598-600. https://doi.org/10.1016/j.jaapos.2011.07.011
Labalette P, Guilbert F, Jourdel D, et al. Bilateral multifocal uveal juvenile xanthogranuloma in a young boy with systemic disease. Graefes Arch Clin Exp Ophthalmol. 2002;240(6):506-9. https://doi.org/10.1007/s00417-002-0465-z
Parmley VC, George DP, Fannin LA. Juvenile xanthogranuloma of the iris in an adult. Arch Ophthalmol. 1998;116(3):377-9. https://doi.org/10.1001/archopht.116.3.377
Sukavatcharin S, Cursino S, Li G, et al. Xanthogranuloma of the iris simulating melanoma in an adult. Am J Ophthalmol. 2007;143(3):529-31. https://doi.org/10.1016/j.ajo.2006.10.023
Karcioglu ZA, Mullaney PB. Diagnosis and management of iris juvenile xanthogranuloma. J Pediatr Ophthalmol Strabismus. 1997;34(1):44-51. https://doi.org/10.3928/0191-3913-19970101-10
##submission.downloads##
Опубліковано
Як цитувати
Номер
Розділ
Ліцензія
Авторське право (c) 2024 Shields M. K., Ferreira L. B., Farrall A. L., Smith J. R.

Ця робота ліцензується відповідно до Creative Commons Attribution 4.0 International License.
Ця робота ліцензується відповідно до ліцензії Creative Commons Attribution 4.0 International (CC BY). Ця ліцензія дозволяє повторно використовувати, поширювати, переробляти, адаптувати та будувати на основі матеріалу на будь-якому носії або в будь-якому форматі за умови обов'язкового посилання на авторів робіт і первинну публікацію у цьому журналі. Ліцензія дозволяє комерційне використання.
ПОЛОЖЕННЯ ПРО АВТОРСЬКІ ПРАВА
Автори, які подають матеріали до цього журналу, погоджуються з наступними положеннями:
- Автори отримують право на авторство своєї роботи одразу після її публікації та назавжди зберігають це право за собою без жодних обмежень.
- Дата початку дії авторського права на статтю відповідає даті публікації випуску, до якого вона включена.
ПОЛІТИКА ДЕПОНУВАННЯ
- Редакція журналу заохочує розміщення авторами рукопису статті в мережі Інтернет (наприклад, у сховищах установ або на особистих веб-сайтах), оскільки це сприяє виникненню продуктивної наукової дискусії та позитивно позначається на оперативності і динаміці цитування.
- Автори мають право укладати самостійні додаткові угоди щодо неексклюзивного розповсюдження статті у тому вигляді, в якому вона була опублікована цим журналом за умови збереження посилання на первинну публікацію у цьому журналі.
- Дозволяється самоархівування постпринтів (версій рукописів, схвалених до друку в процесі рецензування) під час їх редакційного опрацювання або опублікованих видавцем PDF-версій.
- Самоархівування препринтів (версій рукописів до рецензування) не дозволяється.