Our experience in the diagnosis and treatment of peripheral exudative hemorrhagic chorioretinopathy
DOI:
https://doi.org/10.31288/oftalmolzh202451014Keywords:
peripheral exudative hemorrhagic chorioretinopathy, polypoidal choroidal vasculopathy, hemorrhagic detachment of the pigment epitheliumAbstract
Purpose: To present our experience in the examination and treatment of patients with peripheral exudative hemorrhagic chorioretinopathy (PEHCR).
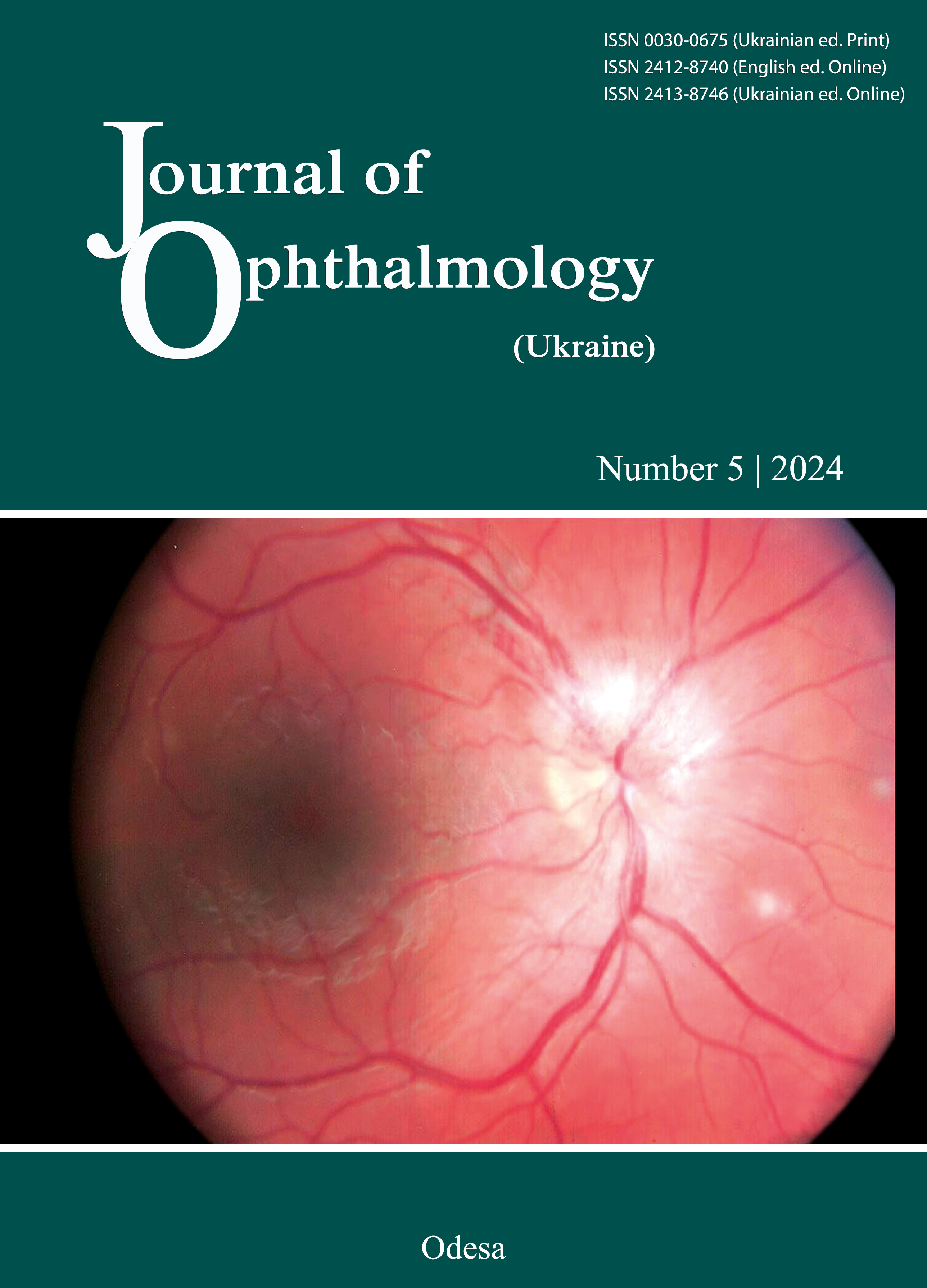
Material and Methods: We retrospectively reviewed the medical records of patients who were finally clinically diagnosed with PEHCR in the 2022-2023 period. History was collected and patients underwent ophthalmological examination including visual acuity, slit-lamp biomicroscopy, color fundus photography, fluorescein angiography and ocular ultrasound. All patients were treated with intravitreal anti-vascular endothelial growth factor (VEGF) therapy. One patient underwent vitreoretinal surgery.
Results: PEHCR was diagnosed in 11 patients (13 eyes), including two patients diagnosed with bilateral lesions. Clinical signs identified included a dome-shaped hemorrhagic detachment of the peripheral retinal pigment epithelium (RPE) with massive exudations. One patient underwent vitreoretinal surgery for vitreoretinal hemorrhage. On B-scan ultrasonography, the PEHCR lesion commonly presented as a dome or plateau-shaped mass with hollow or solid acoustic quality. Ten patients were treated with intravitreal aflibercept.
Conclusion: PEHCR is a chronic disease commonly associated with AMD. Detachment of the peripheral RPE is a major clinical manifestation of the disease, and may be complicated by sub-RPE hemorrhage in early disease. Anti-VEGF therapy is a major method of treatment whereas vitreoretinal surgery is indicated in complications accompanied by massive intravitreal hemorrhage or macula-threatening subretinal hemorrhage. Further investigation is needed to elucidate the etiology and pathogenesis of this entity and demonstrate the efficacy and safety of the aforementioned treatment modalities for PEHCR.
References
Reese AB, Jones IS. Hematomas under the retinal pigment epithelium. Trans Am Ophthalmol Soc.1961;59:43-69.
Shields JA, Augsburger JJ, Brown GC, Stephens RF. The differential diagnosis of posterior uveal melanoma. Ophthalmology.1980;87(6):518-522. https://doi.org/10.1016/S0161-6420(80)35201-9
Shields JA, Mashayekhi A, Ra S, Shields CL. Pseudomelanomas of the posterior uveal tract: the 2006 Taylor R. Smith Lecture. Retina. 2005;25(6):767-771. https://doi.org/10.1097/00006982-200509000-00013
Annesley WH. Peripheral exudative hemorrhagic chorioretinopathy. Trans Am Ophthalmol Soc.1980;78:321.
Silva VB, Brockhurst RJ. Hemorrhagic detachment of the peripheral retinal pigment epithelium. Arch Ophthalmol.1976;94:1295-1300. https://doi.org/10.1001/archopht.1976.03910040167009
Shields CL, Salazar PF, Mashayekhi A, Shields JA. Peripheral exudative hemorrhagic chorioretinopathy simulating choroidal melanoma in 173 eyes. Ophthalmology. 2009;116(3):529-535. https://doi.org/10.1016/j.ophtha.2008.10.015
Rishi P, Das A, Sarate P, Rishi E. Management of peripheral polypoidal choroidal vasculopathy with intravitreal bevacizumab and indocyanine green angiography-guided laser photocoagulation. Indian J Ophthalmol.2012;60(1):60-63. https://doi.org/10.4103/0301-4738.91351
Goldman DR, Freund KB, McCannel CA, Sarraf D. Peripheral polypoidal choroidal vasculopathy as a cause of peripheral exudative hemorrhagic chorioretinopathy: a report of 10 eyes. Retina. 2013;33(1):48-55. https://doi.org/10.1097/IAE.0b013e31825df12a
Venkatesh R, Mishra P, Nahata H, Reddy NG, Yadav NK, Chhablani J. Peripheral and macular polypoidal choroidal vasculopathy: A retrospective comparative case series. European Journal of Ophthalmology. 2023;33(1):448-454. https://doi.org/10.1177/11206721221100624
Bloome MA, Ruiz RS. Massive spontaneous subretinal hemorrhage. Am J Ophthalmol. 1978;86:630-637. https://doi.org/10.1016/0002-9394(78)90181-2
Delaney WV Jr, Torrisi PF, Hampton GR, Seigart CR, Hay PB. Hemorrhagic peripheral pigment pithelial disease. Arch Ophthalmol. 1988;106:646-650. https://doi.org/10.1001/archopht.1988.01060130700028
Kingham JD. Hemorrhagic detachment of the peripheral retinal pigment epithelium. Ann Ophthalmol. 1978;10:175- 178.
Potter JW, Semes LP. Hemorrhagic detachment of the peripheral retinal pigment epithelium. Am J Optom Physiol Opt. 1985;62:161-164. https://doi.org/10.1097/00006324-198503000-00002
Bardenstein DS, Char DH, Irvine AR, Stone RD. Extramacular disciform lesions simulating uveal tumors. Ophthalmology. 1992;99:944-951. https://doi.org/10.1016/S0161-6420(92)31870-6
Bec P, Secheyron P, Arne JL, Aubry JP. La néovascularisation sous-rétinienne périphérique et ses conséquences pathologiques. J Fr Ophtalmol. 1979;2:329-336.
Vine AK, Johnson MW. Peripheral choroidal neovascularization. Eur J Ophthalmol. 1996;6:44-49. https://doi.org/10.1177/112067219600600110
Shroff D, Sharma M, Chhablani J, Gupta P, Gupta C, Shroff C. Peripheral exudative hemorrhagic chorioretinopathy-a new addition to the spectrum of pachychoroid disease?. Retina. 2021;41(7):1518-1525. https://doi.org/10.1097/IAE.0000000000003063
Yamashiro K, Yanagi Y, Koizumi H, Matsumoto H, CheungCMG, Gomi F,et al. Relationship between Pachychoroid and Polypoidal Choroidal Vasculopathy. J Clin Med. 2022;11(15):4614. https://doi.org/10.3390/jcm11154614
Mantel I, Uffer S, Zografos L. Peripheral exudative hemorrhagic chorioretinopathy: A clinical, angiographic, and histologic study. Am J Ophthalmol. 2009;148:932-938. https://doi.org/10.1016/j.ajo.2009.06.032
John A, Gonzales Kapil G, KapoorSyed K. Gibran Peripheral Exudative Hemorrhagic Chorioretinopathy: A Clinical, Angiographic, and Histologic Study. American Journal of Ophthalmology.2010;149(6):1013-1014. https://doi.org/10.1016/j.ajo.2010.02.018
Gonzales JA, Kapoor KJ, Gibran SK. Peripheral Exudative Hemorrhagic Chorioretinopathy: A Clinical, Angiographic, and Histologic Study. Am J Ophthalmol. 2010 Jun;149(6):1013-4. https://doi.org/10.1016/j.ajo.2010.02.018
Pinarci EY, Kilic I, Bayar SA, Sizmaz S, Akkoyun I, Yilmaz G. Clinical characteristics of peripheral exudative hemorrhagic chorioretinopathy and its response to bevacizumab therapy. Eye.2013;27(1):111-2. https://doi.org/10.1038/eye.2012.239
Gonzales JA, Kapoor KG, Gibran SK. Peripheral exudative hemorrhagic chorioretinopathy: a clinical, angiographic, and histologic study, comment on. Am J Ophthalmol. 2010;149(6):1013-4. https://doi.org/10.1016/j.ajo.2010.02.018
Barkmeier AJ, Kadikoy H, Holz ER, Carvounis PE. Regression of serous macular detachment due to peripheral exudative hemorrhagic chorioretinopathy following intravitreal bevacizumab. Eur J Ophthalmol.2011;21(4):506-8. https://doi.org/10.5301/EJO.2011.6246
Takkar B, Roy S, Sodhi PK, Azad S, Bajwa GS. Peripheral choroidal neovascular membrane in a case of peripheral exudative hemorrhagic chorioretinopathy managed with combination therapy. Int Ophthalmol.2017;37:429-431. https://doi.org/10.1007/s10792-016-0277-5
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Nasinnyk I.O., Levytska G.V., Umanets, M.M.

This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International (CC BY 4.0) that allows users to read, download, copy, distribute, print, search, or link to the full texts of the articles, or use them for any other lawful purpose, without asking prior permission from the publisher or the author as long as they cite the source.
COPYRIGHT NOTICE
Authors who publish in this journal agree to the following terms:
- Authors hold copyright immediately after publication of their works and retain publishing rights without any restrictions.
- The copyright commencement date complies the publication date of the issue, where the article is included in.
DEPOSIT POLICY
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) during the editorial process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work with an acknowledgement of its initial publication in this journal.
- Post-print (post-refereeing manuscript version) and publisher's PDF-version self-archiving is allowed.
- Archiving the pre-print (pre-refereeing manuscript version) not allowed.