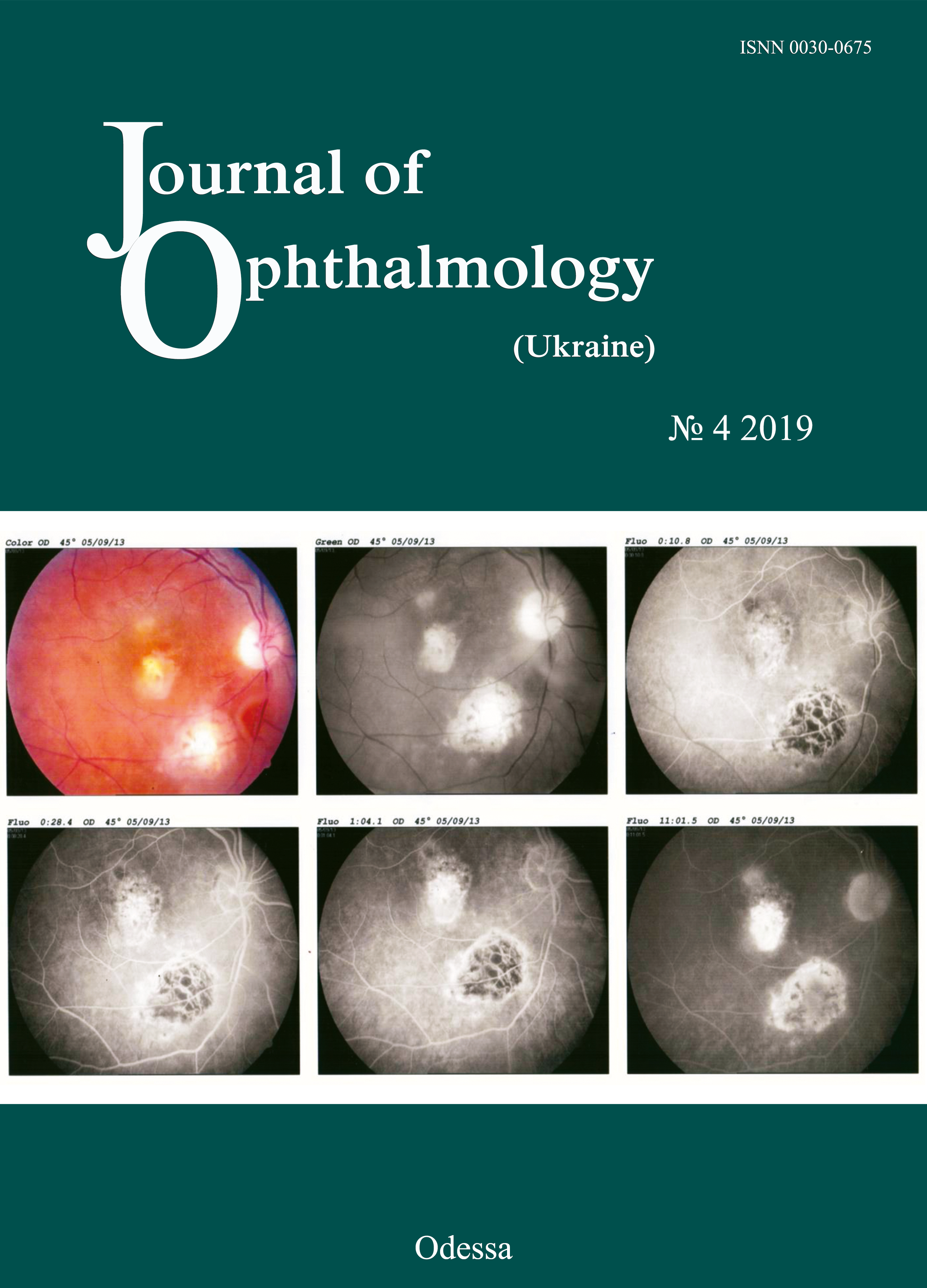
Визуализация внутриглазных инородных тел, расположенных в проекции цилиарного тела, способом инфракрасной диафаноскопии
DOI:
https://doi.org/10.31288/oftalmolzh201942327Ключові слова:
проникающее ранение глазного яблока, внутриглазное инородное тело, инфракрасное излучение, диафаноскопияАнотація
Актуальность. Несмотря на совершенствование диагностических технологий, проблема обнаружения внутриглазных инородных тел (ВИТ), расположенных в проекции цилиарного тела, остается одной из актуальных задач офтальмотравматологии.
Цель. Изучить возможность визуализации внутриглазных инородных тел в проекции цилиарного тела способом транспальпебральной инфракрасной диафаноскопии.
Материал и методы. Под наблюдением находились 10 пациентов (10 глаз, все мужчины в возрасте от 20 - 45 лет) с проникающим ранением глазного яблока и наличием ВИТ. Во всех случаях были выполнены: рентгендиагностика, ультразвуковое сканирование переднего и заднего отделов глазного яблока, ультразвуковая дистанционная биометрия, металлодетекция, а также инфракрасная транспальпебральная диафаноскопия.
Результаты. У всех больных способом инфракрасной транспальпебральной диафаноскопии на склере были визуализированы тени структур цилиарного тела (плоской и отростчатой его частей), а также тень ВИТ. Во всех случаях была определена локализация ВИТ по отношению к структурам цилиарного тела.
Вывод. Способ инфракрасной транспальпебральной диафаноскопии у больных с проникающим ранением глазного яблока позволяет неинвазивно визуализировать ВИТ, расположенные в проекции цилиарного тела, и определить их локализацию по отношению к структурам цилиарного тела.
Посилання
1.Erikitola O, Shahid S, Waqar S, Hewick S. Ocular trauma: classification, management and prognosis. Brit J Hosp Med. 2013;74:108-11. https://doi.org/10.12968/hmed.2013.74.Sup7.C108
2.Loporchio D, Mukkamala L, Gorukanti K, Zarbin M, Langer P, Bhagat N. Intraocular foreign bodies. Surv Ophthalmol. 2016; 61(5):582-96.https://doi.org/10.1016/j.survophthal.2016.03.005
3.Lima-G?mez V, Blanco-Hern?ndez D, Rojas-Dosal J. Ocular trauma score at the initial evaluation of ocular trauma.CIR CIR. 2010 May-Jun;78(3):209-13.
4.Arora R, Sanga L, Kumar M, Taneja M. Intralenticular foreign bodies: report ofeight cases and review of management. Indian J Ophthalmol. 2000;48:119-22.
5.Zhang Y, Zhang M, Jiang C, Qiu HY. Intraocular foreign bodies in Сhina: clinical characteristics, prognostic factors, and visual outcomes in 1,421 eyes. Am J Ophthalmol. 2011;152(1):66-73.https://doi.org/10.1016/j.ajo.2011.01.014
6.Raina U, Kumar V, Kumar V, Sud R, Goel N, Ghosh B. Metallic intraocular foreignbody retained for four years - an unusual presentation. Cont Lens Anterior Eye. 2010;33:202-4.https://doi.org/10.1016/j.clae.2010.01.005
7.Gundorova RA, Stepanov AV, Kurbanova NF. [Current ocular traumatology]. Moscow: Meditsina; 2007. Russian.
8.Pandey A.N. Ocular Foreign Bodies: A Review. J Clin Exp Ophthalmol. 2017; 8: 645.https://doi.org/10.4172/2155-9570.1000645
9.Gundarova R, Chentsova E, Leparskaya N, Lugovkina K, Pavlova V, Shaldin P. [Ultrasound biomicroscopy and laser Doppler fluormetry study of the ciliary body in traumatic retinal detachment due to ocular contusion]. Rus Ophthalmol J. 2012;3:14-8. Russian.
10.Kaushik S, Ichhpujani P, Ramasubramanian A, Pandav SS. Occult intraocular foreign body: ultrasound biomicroscopy holds the key. Int Ophthalmol. 2008;28:71-3.https://doi.org/10.1007/s10792-007-9110-5
11.Koch FHJ, Deuchler S, Singh P, Hessling M. Diaphanoskopie am Auge. Ophthalmologe. 2017;114(9):857-64.https://doi.org/10.1007/s00347-017-0470-6
12.Zadorozhnyy O, Alibet Yassine, Kryvoruchko A, Levytska G, Pasyechnikova N. Dimensions of ciliary body structures in various axial lengths in patients with rhegmatogenous retinal detachment. Journal of Ophthalmology (Ukraine). 2017;6:32-6.https://doi.org/10.31288/oftalmolzh201763236
13.Zadorozhnyy O, Korol A, Nevska A, Kustryn T, Pasyechnikova N. Ciliary body imaging with transpalpebral near-infrared transillumination - a pilot study. Klinika oczna. 2016;3:184-6.
14.Wylegala E, Dobrowolski D, Nowinska A, Tarnawska D. Anterior segment optical coherence tomography in eye injuries. Graef Arch Clin. Exp.2009;247:451-5.https://doi.org/10.1007/s00417-008-0937-x
15.Pasyechnikova N, Naumenko V, Korol A, Zadorozhnyy O. Digital imaging of the fundus with long-wave illumination. Klinika oczna. 2009;111(1-3):18-20.
##submission.downloads##
Опубліковано
Як цитувати
Номер
Розділ
Ліцензія
Авторське право (c) 2025 М. Б. Коган, О. С. Задорожный, О. С. Петрецкая, Т. А. Красновид, А. Р. Король, Н.В. Пасечникова

Ця робота ліцензується відповідно до Creative Commons Attribution 4.0 International License.
Ця робота ліцензується відповідно до ліцензії Creative Commons Attribution 4.0 International (CC BY). Ця ліцензія дозволяє повторно використовувати, поширювати, переробляти, адаптувати та будувати на основі матеріалу на будь-якому носії або в будь-якому форматі за умови обов'язкового посилання на авторів робіт і первинну публікацію у цьому журналі. Ліцензія дозволяє комерційне використання.
ПОЛОЖЕННЯ ПРО АВТОРСЬКІ ПРАВА
Автори, які подають матеріали до цього журналу, погоджуються з наступними положеннями:
- Автори отримують право на авторство своєї роботи одразу після її публікації та назавжди зберігають це право за собою без жодних обмежень.
- Дата початку дії авторського права на статтю відповідає даті публікації випуску, до якого вона включена.
ПОЛІТИКА ДЕПОНУВАННЯ
- Редакція журналу заохочує розміщення авторами рукопису статті в мережі Інтернет (наприклад, у сховищах установ або на особистих веб-сайтах), оскільки це сприяє виникненню продуктивної наукової дискусії та позитивно позначається на оперативності і динаміці цитування.
- Автори мають право укладати самостійні додаткові угоди щодо неексклюзивного розповсюдження статті у тому вигляді, в якому вона була опублікована цим журналом за умови збереження посилання на первинну публікацію у цьому журналі.
- Дозволяється самоархівування постпринтів (версій рукописів, схвалених до друку в процесі рецензування) під час їх редакційного опрацювання або опублікованих видавцем PDF-версій.
- Самоархівування препринтів (версій рукописів до рецензування) не дозволяється.