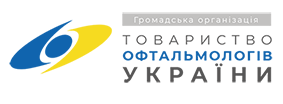
Фотобіомодуляційна терапія в офтальмології
DOI:
https://doi.org/10.31288/oftalmolzh202254753Ключові слова:
фотобіомодуляційна терапія, світло червоного та інфрачервоного діапазону, сітківка, мітохондріїАнотація
Фотобіомодуляційна терапія поєднує лікувальні підходи із застосуванням неіонізуючих джерел світлового випромінювання видимого та ближнього інфрачервоного діапазону спектру, які забезпечують нетеплові фотохімічні реакції у різних біологічних структурах. У роботі викладено накопичений у різних сферах медицини, включаючи офтальмологію, експериментальний та клінічний досвід використання відомих механізмів фотобіомодуляційного впливу на клітини та тканини.
Посилання
1. Anders JJ, Lanzafame RJ, Arany PR. Low-level light/laser therapy versus photobiomodulation therapy. Photomed Laser Surg. 2015;33(4):183-184. doi:10.1089/pho.2015.9848 https://doi.org/10.1089/pho.2015.9848
2. Karu TI. Effects of visible radiation on cultured cells. Photochem Photobiol. 1990;52(6):1089-1098. doi:10.1111/j.1751-1097.1990.tb08450.x https://doi.org/10.1111/j.1751-1097.1990.tb08450.x
3. Geneva II. Photobiomodulation for the treatment of retinal diseases: a review. Int J Ophthalmol. 2016;9(1):145-152. doi:10.18240/ijo.2016.01.24 https://doi.org/10.18240/ijo.2016.01.24
4. Mester E, Szende B, Gärtner P. Die Wirkung der Lasstrahlen auf den Haarwuchs der Maus [The effect of laser beams on the growth of hair in mice]. Radiobiol Radiother (Berl). 1968;9(5):621-626.
5. Kovács IB, Mester E, Görög P. Stimulation of wound healing with laser beam in the rat. Experientia. 1974;30(11):1275-1276. doi:10.1007/BF01945182 https://doi.org/10.1007/BF01945182
6. Linnik LA, Usov NI, Chechin PP, Pelepchuk OS. Perspektivy ispol'zovaniia stimuliruiushcheĭ lazernoĭ terapii v oftal'mologii [Prospects for using stimulating laser therapy in ophthalmology]. Oftalmol Zh. 1982;37(4):193-7. Russian. PMID: 7145299.
7. Linnik LA. Lazernaia terapiia v oftal'mologii [Laser therapy in ophthalmology]. Oftalmol Zh. 1985;(8):451-5. Russian. PMID: 4088581.
8. Karu T, Pyatibrat L, Kalendo G. Irradiation with He-Ne laser increases ATP level in cells cultivated in vitro. J Photochem Photobiol B. 1995;27(3):219-223. doi:10.1016/1011-1344(94)07078-3 https://doi.org/10.1016/1011-1344(94)07078-3
9. Manteifel V, Bakeeva L, Karu T. Ultrastructural changes in chondriome of human lymphocytes after irradiation with He-Ne laser: appearance of giant mitochondria. J Photochem Photobiol B. 1997;38(1):25-30. doi:10.1016/s1011-1344(96)07426-x https://doi.org/10.1016/S1011-1344(96)07426-X
10. Sutherland JC. Biological effects of polychromatic light. Photochem Photobiol. 2002;76(2):164-170. doi:10.1562/0031-8655(2002)076<0164:beopl>2.0.co;2 https://doi.org/10.1562/0031-8655(2002)076<0164:BEOPL>2.0.CO;2
11. Kato M, Shinizawa K, Yoshikawa S. Cythochrome oxidase is a possible photoreceptor in mitochondria. Photobiochem Photobiophys. 1981;2:263-269 https://doi.org/10.1016/S0165-8646(24)00252-6
12. Greco M, Guida G, Perlino E, Marra E, Quagliariello E. Increase in RNA and protein synthesis by mitochondria irradiated with helium-neon laser. Biochem Biophys Res Commun. 1989;163(3):1428-1434. doi:10.1016/0006-291x(89)91138-8 https://doi.org/10.1016/0006-291X(89)91138-8
13. Karu T. Primary and secondary mechanisms of action of visible to near-IR radiation on cells. J Photochem Photobiol B. 1999;49(1):1-17. doi:10.1016/S1011-1344(98)00219-X https://doi.org/10.1016/S1011-1344(98)00219-X
14. Passarella S, Casamassima E, Molinari S, et al. Increase of proton electrochemical potential and ATP synthesis in rat liver mitochondria irradiated in vitro by helium-neon laser. FEBS Lett. 1984;175(1):95-99. doi:10.1016/0014-5793(84)80577-3 https://doi.org/10.1016/0014-5793(84)80577-3
15. Karu TI, Kolyakov SF. Exact action spectra for cellular responses relevant to phototherapy. Photomed Laser Surg. 2005;23(4):355-361. doi:10.1089/pho.2005.23.355 https://doi.org/10.1089/pho.2005.23.355
16. Hawkins D, Abrahamse H. Biological effects of helium-neon laser irradiation on normal and wounded human skin fibroblasts. Photomed Laser Surg. 2005;23(3):251-259. doi:10.1089/pho.2005.23.251 https://doi.org/10.1089/pho.2005.23.251
17. Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR. The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng. 2012;40(2):516-533. doi:10.1007/s10439-011-0454-7 https://doi.org/10.1007/s10439-011-0454-7
18. Capaldi RA, Malatesta F, Darley-Usmar VM. Structure of cytochrome c oxidase. Biochim Biophys Acta. 1983;726(2):135-148. doi:10.1016/0304-4173(83)90003-4 https://doi.org/10.1016/0304-4173(83)90003-4
19. Quirk BJ, Whelan HT. What Lies at the Heart of Photobiomodulation: Light, Cytochrome C Oxidase, and Nitric Oxide - Review of the Evidence. Photobiomodulation, Photomedicine, and Laser Surgery. 2020;38(9);527-530. https://doi.org/10.1089/photob.2020.4905
20. Karu TI, Pyatibrat LV, Kolyakov SF, Afanasyeva NI. Absorption measurements of a cell monolayer relevant to phototherapy: reduction of cytochrome c oxidase under near IR radiation. J Photochem Photobiol B. 2005;81(2):98-106. https://doi.org/10.1016/j.jphotobiol.2005.07.002
21. Wong-Riley MT, Liang HL, Eells JT, et al. Photobiomodulation directly benefits primary neurons functionally inactivated by toxins: role of cytochrome c oxidase. J Biol Chem. 2005;280(6):4761-4771. https://doi.org/10.1074/jbc.M409650200
22. Karu TI, Pyatibrat LV, Afanasyeva NI. A novel mitochondrial signaling pathway activated by visible-to-near infrared radiation. Photochem Photobiol. 2004;80(2):366-372. https://doi.org/10.1562/2004-03-25-RA-123
23. Lovschall H, Arenholt-Bindslev D. Low level laser therapy effect on mitochondrial rhodamine 123 uptake in human oral fibroblasts in vitro. Lasers Life Sci. 1998;8:101-116
24. Moore P, Ridgway TD, Higbee RG, Howard EW, Lucroy MD. Effect of wavelength on low-intensity laser irradiation-stimulated cell proliferation in vitro. Lasers Surg Med. 2005;36(1):8-12. doi:10.1002/lsm.20117 https://doi.org/10.1002/lsm.20117
25. Hawkins D, Houreld N, Abrahamse H. Low level laser therapy (LLLT) as an effective therapeutic modality for delayed wound healing. Ann N Y Acad Sci. 2005;1056:486-493. doi:10.1196/annals.1352.040 https://doi.org/10.1196/annals.1352.040
26. Yu HS, Wu CS, Yu CL, Kao YH, Chiou MH. Helium-neon laser irradiation stimulates migration and proliferation in melanocytes and induces repigmentation in segmental-type vitiligo. J Invest Dermatol. 2003;120(1):56-64. doi:10.1046/j.1523-1747.2003.12011.x https://doi.org/10.1046/j.1523-1747.2003.12011.x
27. Lohr NL, Keszler A, Pratt P, Bienengraber M, Warltier DC, Hogg N. Enhancement of nitric oxide release from nitrosyl hemoglobin and nitrosyl myoglobin by red/near infrared radiation: potential role in cardioprotection. J Mol Cell Cardiol. 2009;47(2):256-263.
https://doi.org/10.1016/j.yjmcc.2009.03.009
28. Shiva S, Gladwin MT. Shining a light on tissue NO stores: near infrared release of NO from nitrite and nitrosylated hemes. J Mol Cell Cardiol. 2009;46(1):1-3. https://doi.org/10.1016/j.yjmcc.2008.10.005
29. Antunes F, Boveris A, Cadenas E. On the mechanism and biology of cytochrome oxidase inhibition by nitric oxide. Proc Natl Acad Sci U S A. 2004;101(48):16774-16779. https://doi.org/10.1073/pnas.0405368101
30. Mitchell UH, Mack GL. Low-level laser treatment with near-infrared light increases venous nitric oxide levels acutely: a single-blind, randomized clinical trial of efficacy. Am J Phys Med Rehabil. 2013;92(2):151-156. https://doi.org/10.1097/PHM.0b013e318269d70a
31. Nawashiro H, Wada K, Nakai K, Sato S. Focal increase in cerebral blood flow after treatment with near-infrared light to the forehead in a patient in a persistent vegetative state. Photomed Laser Surg. 2012;30(4):231-233. https://doi.org/10.1089/pho.2011.3044
32. Liang HL, Whelan HT, Eells JT, Wong-Riley MT. Near-infrared light via light-emitting diode treatment is therapeutic against rotenone- and 1-methyl-4-phenylpyridinium ion-induced neurotoxicity. Neuroscience. 2008;153(4):963-974. https://doi.org/10.1016/j.neuroscience.2008.03.042
33. Ying R, Liang HL, Whelan HT, Eells JT, Wong-Riley MT. Pretreatment with near-infrared light via light-emitting diode provides added benefit against rotenone- and MPP+-induced neurotoxicity. Brain Res. 2008;1243:167-173. https://doi.org/10.1016/j.brainres.2008.09.057
34. Salehpour F, Farajdokht F, Cassano P, et al. Near-infrared photobiomodulation combined with coenzyme Q10 for depression in a mouse model of restraint stress: reduction in oxidative stress, neuroinflammation, and apoptosis. Brain Res Bull. 2019;144:213-222.
https://doi.org/10.1016/j.brainresbull.2018.10.010
35. Wong-Riley MT. Energy metabolism of the visual system. Eye Brain. 2010;2:99-116. https://doi.org/10.2147/EB.S9078
36. Lock JH, Irani NK, Newman NJ. Neuro-ophthalmic manifestations of mitochondrial disorders and their management. Taiwan J Ophthalmol. 2020;11(1):39-52. Published 2020 Dec 4. https://doi.org/10.4103/tjo.tjo_68_20
37. Albarracin R, Valter K. 670 nm red light preconditioning supports Müller cell function: evidence from the white light-induced damage model in the rat retina. Photochem Photobiol. 2012;88(6):1418-1427. https://doi.org/10.1111/j.1751-1097.2012.01130.x
38. Tang J, Du Y, Lee CA, Talahalli R, Eells JT, Kern TS. Low-intensity far-red light inhibits early lesions that contribute to diabetic retinopathy: in vivo and in vitro. Invest Ophthalmol Vis Sci. 2013;54(5):3681-3690. Published 2013 May 1. https://doi.org/10.1167/iovs.12-11018
39. Fuma S, Murase H, Kuse Y, Tsuruma K, Shimazawa M, Hara H. Photobiomodulation with 670 nm light increased phagocytosis in human retinal pigment epithelial cells. Mol Vis. 2015;21:883-892.
40. Karu TI. Mitochondrial signalling in mammalian cells activated by red and near-IR radiation. Photochem Photobiol. 2008;84(5):1091-1099. https://doi.org/10.1111/j.1751-1097.2008.00394.x
41. Rojas JC, Gonzalez-Lima F. Low-level light therapy of the eye and brain. Eye Brain. 2011;3:49-67. Published 2011 Oct 14. https://doi.org/10.2147/EB.S21391
42. Peplow PV, Chung TY, Baxter GD. Laser photobiomodulation of wound healing: a review of experimental studies in mouse and rat animal models. Photomed Laser Surg. 2010;28(3):291-325. https://doi.org/10.1089/pho.2008.2446
43. Mester E, Nagylucskay S, Doklen A, Tisza S. Laser stimulation of wound healing. Acta Chir Acad Sci Hung. 1976;17:49-55
44. Thomas DW, O'Neill ID, Harding KG, Shepherd JP. Cutaneous wound healing: a current perspective. J Oral Maxillofac Surg. 1995;53(4):442-447. https://doi.org/10.1016/0278-2391(95)90721-1
45. Posten W, Wrone DA, Dover JS, Arndt KA, Silapunt S, Alam M. Low-level laser therapy for wound healing: mechanism and efficacy. Dermatol Surg. 2005;31(3):334-340. https://doi.org/10.1111/j.1524-4725.2005.31086
46. Bisht D, Mehrotra R, Singh PA, Atri SC, Kumar A. Effect of helium-neon laser on wound healing. Indian J Exp Biol. 1999;37(2):187-189.
47. Meyers AD. Lasers and wound healing. Arch Otolaryngol Head Neck Surg. 1990;116:1128.
https://doi.org/10.1001/archotol.1990.01870100022005
48. Skinner SM, Gage JP, Wilce PA, Shaw RM. A preliminary study of the effects of laser radiation on collagen metabolism in cell culture. Aust Dent J. 1996;41(3):188-192. https://doi.org/10.1111/j.1834-7819.1996.tb04854.x
49. Bjordal JM, Couppé C, Chow RT, Tunér J, Ljunggren EA. A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust J Physiother. 2003;49(2):107-116. https://doi.org/10.1016/S0004-9514(14)60127-6
50. Wahl G, Bastänier S. Der Softlaser in der postoperativen Nachsorge bei dentoalveolären Eingriffen [Soft laser in postoperative care in dentoalveolar treatment]. ZWR. 1991;100(8):512-515.
51. Chow RT, Johnson MI, Lopes-Martins RA, Bjordal JM. Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. Lancet. 2009;374(9705):1897-1908.
https://doi.org/10.1016/S0140-6736(09)61522-1
52. Streeter J, De Taboada L, Oron U. Mechanisms of action of light therapy for stroke and acute myocardial infarction. Mitochondrion. 2004;4(5-6):569-576. https://doi.org/10.1016/j.mito.2004.07.037
53. Oron U, Yaakobi T, Oron A, et al. Low-energy laser irradiation reduces formation of scar tissue after myocardial infarction in rats and dogs. Circulation. 2001;103(2):296-301. https://doi.org/10.1161/01.CIR.103.2.296
54. Yaakobi T, Shoshany Y, Levkovitz S, Rubin O, Ben Haim SA, Oron U. Long-term effect of low energy laser irradiation on infarction and reperfusion injury in the rat heart. J Appl Physiol (1985). 2001;90(6):2411-2419. https://doi.org/10.1152/jappl.2001.90.6.2411
55. Oron U, Yaakobi T, Oron A, et al. Attenuation of infarct size in rats and dogs after myocardial infarction by low-energy laser irradiation. Lasers Surg Med. 2001;28(3):204-211. https://doi.org/10.1002/lsm.1039
56. Lee G, Ikeda RM, Dwyer RM, Hussein H, Dietrich P, Mason DT. Feasibility of intravascular laser irradiation for in vivo visualization and therapy of cardiocirculatory diseases. Am Heart J. 1982;103(6):1076-1077. https://doi.org/10.1016/0002-8703(82)90576-2
57. Wong-Riley MT, Bai X, Buchmann E, Whelan HT. Light-emitting diode treatment reverses the effect of TTX on cytochrome oxidase in neurons. Neuroreport. 2001;12(14):3033-3037. https://doi.org/10.1097/00001756-200110080-00011
58. Hashmi JT, Huang YY, Osmani BZ, Sharma SK, Naeser MA, Hamblin MR. Role of low-level laser therapy in neurorehabilitation. PM R. 2010;2(12 Suppl 2):S292-S305. https://doi.org/10.1016/j.pmrj.2010.10.013
59. Liang HL, Whelan HT, Eells JT, et al. Photobiomodulation partially rescues visual cortical neurons from cyanide-induced apoptosis. Neuroscience. 2006;139(2):639-649. https://doi.org/10.1016/j.neuroscience.2005.12.047
60. Naeser MA, Saltmarche A, Krengel MH, Hamblin MR, Knight JA. Improved cognitive function after transcranial, light-emitting diode treatments in chronic, traumatic brain injury: two case reports. Photomed Laser Surg. 2011;29(5):351-358. https://doi.org/10.1089/pho.2010.2814
61. Fitzgerald M, Hodgetts S, Van Den Heuvel C, et al. Red/near-infrared irradiation therapy for treatment of central nervous system injuries and disorders. Rev Neurosci. 2013;24(2):205-226. https://doi.org/10.1515/revneuro-2012-0086
62. Uozumi Y, Nawashiro H, Sato S, Kawauchi S, Shima K, Kikuchi M. Targeted increase in cerebral blood flow by transcranial near-infrared laser irradiation. Lasers Surg Med. 2010;42(6):566-576. https://doi.org/10.1002/lsm.20938
63. Rojas JC, Lee J, John JM, Gonzalez-Lima F. Neuroprotective effects of near-infrared light in an in vivo model of mitochondrial optic neuropathy. J Neurosci. 2008;28(50):13511-13521. https://doi.org/10.1523/JNEUROSCI.3457-08.2008
64. Lapchak PA, Salgado KF, Chao CH, Zivin JA. Transcranial near-infrared light therapy improves motor function following embolic strokes in rabbits: an extended therapeutic window study using continuous and pulse frequency delivery modes. Neuroscience. 2007;148(4):907-914. https://doi.org/10.1016/j.neuroscience.2007.07.002
65. Oron A, Oron U, Chen J, et al. Low-level laser therapy applied transcranially to rats after induction of stroke significantly reduces long-term neurological deficits. Stroke. 2006;37(10):2620-2624. https://doi.org/10.1161/01.STR.0000242775.14642.b8
66. Detaboada L, Ilic S, Leichliter-Martha S, Oron U, Oron A, Streeter J. Transcranial application of low-energy laser irradiation improves neurological deficits in rats following acute stroke. Lasers Surg Med. 2006;38(1):70-73. https://doi.org/10.1002/lsm.20256
67. Lampl Y, Zivin JA, Fisher M, et al. Infrared laser therapy for ischemic stroke: a new treatment strategy: results of the NeuroThera Effectiveness and Safety Trial-1 (NEST-1). Stroke. 2007;38(6):1843-1849. https://doi.org/10.1161/STROKEAHA.106.478230
68. Moges H, Vasconcelos OM, Campbell WW, et al. Light therapy and supplementary Riboflavin in the SOD1 transgenic mouse model of familial amyotrophic lateral sclerosis (FALS). Lasers Surg Med. 2009;41(1):52-59.https://doi.org/10.1002/lsm.20732
69. Zhang L, Xing D, Zhu D, Chen Q. Low-power laser irradiation inhibiting Abeta25-35-induced PC12 cell apoptosis via PKC activation. Cell Physiol Biochem. 2008;22(1-4):215-222. https://doi.org/10.1159/000149799
70. Michalikova S, Ennaceur A, van Rensburg R, Chazot PL. Emotional responses and memory performance of middle-aged CD1 mice in a 3D maze: effects of low infrared light. Neurobiol Learn Mem. 2008;89(4):480-488. https://doi.org/10.1016/j.nlm.2007.07.014
71. Trimmer PA, Schwartz KM, Borland MK, De Taboada L, Streeter J, Oron U. Reduced axonal transport in Parkinson's disease cybrid neurites is restored by light therapy. Mol Neurodegener. 2009;4:26. https://doi.org/10.1186/1750-1326-4-26
72. Shaw VE, Spana S, Ashkan K, et al. Neuroprotection of midbrain dopaminergic cells in MPTP-treated mice after near-infrared light treatment. J Comp Neurol. 2010;518(1):25-40. https://doi.org/10.1002/cne.22207
73. Valla J, Berndt JD, Gonzalez-Lima F. Energy hypometabolism in posterior cingulate cortex of Alzheimer's patients: superficial laminar cytochrome oxidase associated with disease duration. J Neurosci. 2001;21(13):4923-4930. https://doi.org/10.1523/JNEUROSCI.21-13-04923.2001
74. Valla J, Yaari R, Wolf AB, et al. Reduced posterior cingulate mitochondrial activity in expired young adult carriers of the APOE ε4 allele, the major late-onset Alzheimer's susceptibility gene. J Alzheimers Dis. 2010;22(1):307-313. https://doi.org/10.3233/JAD-2010-100129
75. Schiffer F, Johnston AL, Ravichandran C, et al. Psychological benefits 2 and 4 weeks after a single treatment with near infrared light to the forehead: a pilot study of 10 patients with major depression and anxiety. Behav Brain Funct. 2009;5:46. https://doi.org/10.1186/1744-9081-5-46
76. Askalsky P, Iosifescu DV. Transcranial Photobiomodulation For The Management Of Depression: Current Perspectives. Neuropsychiatr Dis Treat. 2019;15:3255-3272. Published 2019 Nov 22. https://doi.org/10.2147/NDT.S188906
77. Anders JJ, Geuna S, Rochkind S. Phototherapy promotes regeneration and functional recovery of injured peripheral nerve. Neurol Res. 2004;26(2):233-239. https://doi.org/10.1179/016164104225013914
78. Gigo-Benato D, Geuna S, Rochkind S. Phototherapy for enhancing peripheral nerve repair: a review of the literature. Muscle Nerve. 2005;31(6):694-701. https://doi.org/10.1002/mus.20305
79. Leavitt M, Charles G, Heyman E, Michaels D. HairMax LaserComb laser phototherapy device in the treatment of male androgenetic alopecia: A randomized, double-blind, sham device-controlled, multicentre trial. Clin Drug Investig. 2009;29(5):283-292.
https://doi.org/10.2165/00044011-200929050-00001
80. Muste JC, Russell MW, Singh RP. Photobiomodulation Therapy for Age-Related Macular Degeneration and Diabetic Retinopathy: A Review. Clin Ophthalmol. 2021;15:3709-3720. https://doi.org/10.2147/OPTH.S272327
81. Jarrett SG, Boulton ME. Consequences of oxidative stress in age-related macular degeneration. Mol Aspects Med. 2012;33(4):399-417. https://doi.org/10.1016/j.mam.2012.03.009
82. Kokkinopoulos I, Colman A, Hogg C, Heckenlively J, Jeffery G. Age-related retinal inflammation is reduced by 670 nm light via increased mitochondrial membrane potential. Neurobiol Aging. 2013;34(2):602-609. https://doi.org/10.1016/j.neurobiolaging.2012.04.014
83. Eells JT. Mitochondrial Dysfunction in the Aging Retina. Biology (Basel). 2019;8(2):31. https://doi.org/10.3390/biology8020031
84. Ennis S, Gibson J, Cree AJ, Collins A, Lotery AJ. Support for the involvement of complement factor I in age-related macular degeneration. Eur J Hum Genet. 2010;18(1):15-16. https://doi.org/10.1038/ejhg.2009.113
85. Begum R, Powner MB, Hudson N, Hogg C, Jeffery G. Treatment with 670 nm light up regulates cytochrome C oxidase expression and reduces inflammation in an age-related macular degeneration model. PLoS One. 2013;8(2):e57828.
https://doi.org/10.1371/journal.pone.0057828
86. Ivandic BT, Ivandic T. Low-level laser therapy improves vision in patients with age-related macular degeneration. Photomed Laser Surg. 2008;26(3):241-245.https://doi.org/10.1089/pho.2007.2132
87. Merry G, Dotson R, Devenyi R, Markowitz SRS. Photobiomodulation as a new treatment for dry age related macular degeneration RESULTS from the Toronto and Oak Ridge Photobimodulation study in AMD (TORPA). Invest Ophthalmol Vis Sci. 2012;53:2049. https://doi.org/10.4016/40525.01
88. Merry GF, Munk MR, Dotson RS, Walker MG, Devenyi RG. Photobiomodulation reduces drusen volume and improves visual acuity and contrast sensitivity in dry age-related macular degeneration. Acta Ophthalmol. 2017;95(4):e270-e277. https://doi.org/10.1111/aos.13354
89. Markowitz SN, Devenyi RG, Munk MR, et al. A double-masked, randomized, sham-controlled, single-center study with photobiomodulation for the treatment of dry age-related macular degeneration. Retina. 2019;40:1471. https://doi.org/10.1097/IAE.0000000000002632
90. Sergienko AM, Dzuba NO, Pekarik OS. Changes of the optic density of the macular pigment after two courses of low-energy light therapy in patients with dry form of age-related macular degeneration. Oftalmol Zh.2014;5:40-44 https://doi.org/10.31288/oftalmolzh201444044
91. Muste JC, Kalur A, Iyer A, Valentim CCS, Singh RP. Photobiomodulation therapy in age-related macular degeneration. Curr Opin Ophthalmol. 2021;32(3):225-232. https://doi.org/10.1097/ICU.0000000000000742
92. Cheng Y, Du Y, Liu H, Tang J, Veenstra A, Kern TS. Photobiomodulation Inhibits Long-term Structural and Functional Lesions of Diabetic Retinopathy. Diabetes. 2018;67(2):291-298. https://doi.org/10.2337/db17-0803
93. Saliba A, Du Y, Liu H, et al. Photobiomodulation Mitigates Diabetes-Induced Retinopathy by Direct and Indirect Mechanisms: Evidence from Intervention Studies in Pigmented Mice. PLoS One. 2015;10(10):e0139003. https://doi.org/10.1371/journal.pone.0139003
94. Tang J, Herda AA, Kern TS. Photobiomodulation in the treatment of patients with non-center-involving diabetic macular oedema [published correction appears in Br J Ophthalmol. 2014 Oct;98(10):1463. Dosage error in article text]. Br J Ophthalmol. 2014;98(8):1013-1015. https://doi.org/10.1136/bjophthalmol-2013-304477
95. Shen W, Teo KYC, Wood JPM, et al. Preclinical and clinical studies of photobiomodulation therapy for macular oedema. Diabetologia. 2020;63(9):1900-1915.https://doi.org/10.1007/s00125-020-05189-2
96. Kim JE, Glassman AR, Josic K, et al. A Randomized Trial of Photobiomodulation Therapy for Center-Involved Diabetic Macular Edema with Good Visual Acuity (Protocol AE). Ophthalmol Retina. 2022;6(4):298-307. https://doi.org/10.1016/j.oret.2021.10.003
97. Ivandic BT, Ivandic T. Low-level laser therapy improves vision in a patient with retinitis pigmentosa. Photomed Laser Surg. 2014;32(3):181-184. https://doi.org/10.1089/pho.2013.3535
98. Scalinci SZ, Valsecchi N, Pacella E, Trovato Battagliola E. Effects of Photo-Biomodulation in Stargardt Disease. Clin Ophthalmol. 2022;16:85-91. https://doi.org/10.2147/OPTH.S344378
99. Ng WSV, Trigano M, Freeman T, et al. New avenues for therapy in mitochondrial optic neuropathies. Therapeutic Advances in Rare Disease. January 2021. https://doi.org/10.1177/26330040211029037
100. Albarracin R, Eells J, Valter K. Photobiomodulation protects the retina from light-induced photoreceptor degeneration. Invest Ophthalmol Vis Sci. 2011;52(6):3582-3592. https://doi.org/10.1167/iovs.10-6664
101. Eells JT, Henry MM, Summerfelt P, et al. Therapeutic photobiomodulation for methanol-induced retinal toxicity. Proc Natl Acad Sci U S A. 2003;100(6):3439-3444. https://doi.org/10.1073/pnas.0534746100
102. Ivandic BT, Ivandic T. Low-level laser therapy improves visual acuity in adolescent and adult patients with amblyopia. Photomed Laser Surg. 2012;30(3):167-171. https://doi.org/10.1089/pho.2011.3089
103. Guzun OV, Boichuk IM, Chechin PP, Khramenko NI, Konovalova NV. Laser Stimulation of Retina and Optic Nerve in Children with Anisometropic Amblyopia. 2019 IEEE 8th International Conference on Advanced Optoelectronics and Lasers (CAOL). 2019,;1-5.
https://doi.org/10.1109/CAOL46282.2019.9019548
104. Schwartz M, Doron A, Erlich M, et al. Effects of low-energy He-Ne laser irradiation on posttraumatic degeneration of adult rabbit optic nerve. Lasers Surg Med. 1987;7(1):51-55. https://doi.org/10.1002/lsm.1900070109
105. Assia E, Rosner M, Belkin M, Solomon A, Schwartz M. Temporal parameters of low energy laser irradiation for optimal delay of post-traumatic degeneration of rat optic nerve. Brain Res. 1989;476(2):205-212. https://doi.org/10.1016/0006-8993(89)91240-7
##submission.downloads##
Опубліковано
Як цитувати
Номер
Розділ
Ліцензія
Авторське право (c) 2025 О. С. Задорожний, А. Р. Король, І. О. Насінник, Т. Б. Кустрін, А. О. Невська, Н. В. Пасєчнікова

Ця робота ліцензується відповідно до Creative Commons Attribution 4.0 International License.
Ця робота ліцензується відповідно до ліцензії Creative Commons Attribution 4.0 International (CC BY). Ця ліцензія дозволяє повторно використовувати, поширювати, переробляти, адаптувати та будувати на основі матеріалу на будь-якому носії або в будь-якому форматі за умови обов'язкового посилання на авторів робіт і первинну публікацію у цьому журналі. Ліцензія дозволяє комерційне використання.
ПОЛОЖЕННЯ ПРО АВТОРСЬКІ ПРАВА
Автори, які подають матеріали до цього журналу, погоджуються з наступними положеннями:
- Автори отримують право на авторство своєї роботи одразу після її публікації та назавжди зберігають це право за собою без жодних обмежень.
- Дата початку дії авторського права на статтю відповідає даті публікації випуску, до якого вона включена.
ПОЛІТИКА ДЕПОНУВАННЯ
- Редакція журналу заохочує розміщення авторами рукопису статті в мережі Інтернет (наприклад, у сховищах установ або на особистих веб-сайтах), оскільки це сприяє виникненню продуктивної наукової дискусії та позитивно позначається на оперативності і динаміці цитування.
- Автори мають право укладати самостійні додаткові угоди щодо неексклюзивного розповсюдження статті у тому вигляді, в якому вона була опублікована цим журналом за умови збереження посилання на первинну публікацію у цьому журналі.
- Дозволяється самоархівування постпринтів (версій рукописів, схвалених до друку в процесі рецензування) під час їх редакційного опрацювання або опублікованих видавцем PDF-версій.
- Самоархівування препринтів (версій рукописів до рецензування) не дозволяється.