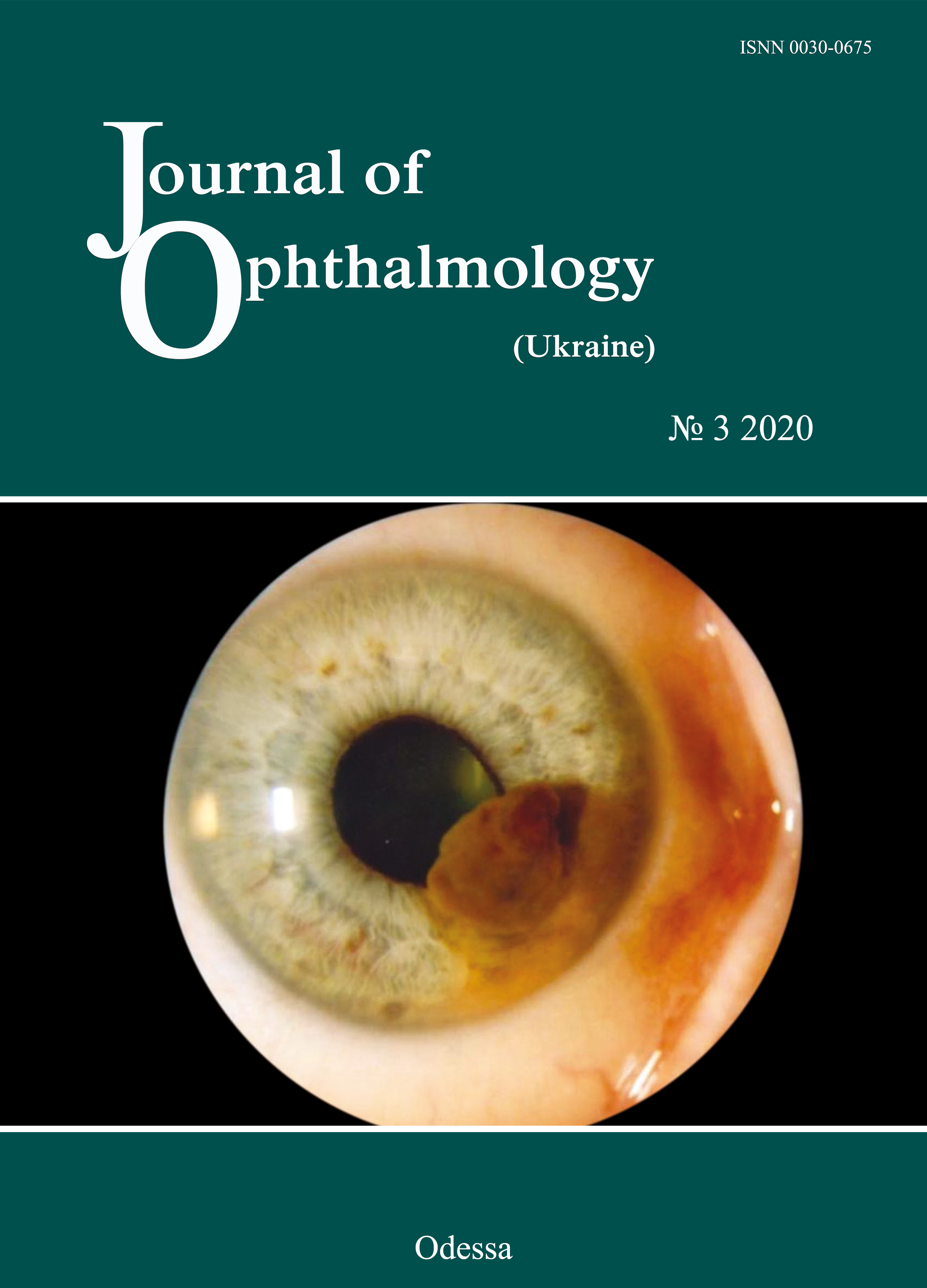
Efficacy of radiowave surgery in the treatment of patients with iris and ciliary body melanoma
DOI:
https://doi.org/10.31288/oftalmolzh202033136Keywords:
uveal melanoma, radiowave surgery unit, treatmentAbstract
Purpose: To determine the efficacy of resecting iris and ciliary body melanoma with the use of a 3.8-4.0-Mhz radiowave surgery unit.
Material and Methods: This study was conducted at Department of Eye Cancer, the Filatov Institute, from 2005 through 2018. The study group involved 45 patients with iris and ciliary body melanoma; the mean age was 56.3 ± 2.2 years, with a slight female predominance (53.3%). Sixty-seven patients who had undergone iridociliary melanoma excision using a conventional technique with cutting tools were used as retrospective controls. The eye examination included visual acuity measurement, perimetry, biomicroscopy and ophthalmoscopy. Tumor, nodus и metastasis (TNM) staging was according to the American Joint Committee on Cancer (AJCC). No metastases were seen at the time of enrollment. The mean tumor prominence at baseline was 4.0 ± 0.3 mm, with a mean base diameter of 8.3 ± 0.4 mm, corresponding to a tumor volume of 34.3 ± 0.7 mm3. All the patients of each group were divided into two subgroups based on baseline visual acuity. The study group involved subgroup 1A (n=37 patients; 82.2%) with a visual acuity of 0.1 to 0.5 and subgroup 1B (n=8 patients; 17.8%) with a visual acuity of 0.6 to 0.8, and the retrospective control group involved subgroup 2A (n=55 patients; 82.1%) with a visual acuity of 0.1 to 0.5 and subgroup 2B (n=12 patients; 17.9%) with a visual acuity of 0.6 to 0.8 (p > 0.05). The analysis was performed by analysis of variance (ANOVA) using Statistica 13.0 (Dell Statsoft Inc., Austin, TX).
Results: The radiosurgical approach to treatment of iridociliary tumors in our patients allowed significantly reducing the rates of intraoperative and postoperative complications (?2=4.16; df=1; p=0.04). In addition, the rates of intraoperative and postoperative complications for the treatment of iridociliary tumors with cutting instruments were 9.1% and 10.4%, respectively. The use of a radiowave surgery unit for uveal melanoma resection allowed preserving baseline visual acuity in all patients, with a tumor recurrence rate of not more than 2.2%.
Conclusion: Early (12-month) treatment outcomes (visual functions and postoperative clinical course) and late treatment outcomes (visual functions; optic media; IOP; and tumor recurrence) for iridociliary melanoma resection using a radiowave 3.8-4.0 MHz unit allow us to state that high-frequency radiowave surgery enables reducing the risk of intraoperative and postoperative complications and, consequently, preserving a good visual function.
References
1.Aronow ME, Topham AK, Singh AD. Uveal Melanoma: 5-Year Update on Incidence, Treatment, and Survival (SEER 1973-2013). Ocul Oncol Pathol. 2018 Apr;4(3):145-151.https://doi.org/10.1159/000480640
2.Papastefanou VP, Cohen VM. Uveal Melanoma. J Skin Cancer. 2011;2011:1-13.https://doi.org/10.1155/2011/573974
3.Shields CL, Kaliki S, Furuta M, et al. American Joint Committee on Cancer Classification of Uveal Melanoma (Anatomic Stage) Predicts Prognosis in 7,731 Patients: The 2013 Zimmerman Lecture. Ophthalmology. 2015 Jun;122(6):1180-6. C https://doi.org/10.1016/j.ophtha.2015.01.026
4.Kim JH, Shin SJ, Heo SJ, et al. Prognoses and Clinical Outcomes of Primary and Recurrent Uveal Melanoma. Cancer Res Treat. 2017 Dec 28. doi: 10.4143/crt.2017.534. https://doi.org/10.4143/crt.2017.534
5.Chua V, Aplin AE. Novel therapeutic strategies and targets in advanced uveal melanoma. Curr Opin Oncol. 2018 Mar;30(2):134-41.https://doi.org/10.1097/CCO.0000000000000425
6.Khomiakova OV, Vit VV, Maletskyi AP. [Comparing structural changes in the rabbit's uveal tract after the use of a radiowave surgery unit versus a cutting tool]. J Ophthalmol (Ukraine). 2019;4:43-48. Ukrainian.
7.Ministry of Health of Ukraine. [Order of Ministry of Health of Ukraine No. 117 "On Approval of Protocols for Provision of Medical Care to Patients with Eye Disease"]. Kyiv, Ukraine; 15 March 2007. https://zakononline.com.ua/documents/show/107241___107241
8.Rebrova OIu. [Statistical analysis of medical data. Application of STATISTICA software package]. Moscow: MediaSfera. 2002. Russian.
9.Smoliakova GP, Pikhovskaia IG, Luz'ianina IG, Sorokin EL. [Method for radiosurgical treatment of uveal melanoblastoma]. Patent of Russian Federation RU No. 2265423 A61F dated 10.09.2006. Patent owner: Far East State Medical University. Application filed on 20.02.2005. Information Bulletin No. 34 issued 10.12.2005.
10.Yang J, Manson DK, Marr BP, Carvajal RD. Treatment of uveal melanoma: where are we now? Ther Adv Med Oncol. 2018 Feb 21;10:1758834018757175.https://doi.org/10.1177/1758834018757175
11.Uveal Melanoma. Available at: https://eyewiki.aao.org/Uveal_Melanoma#targetText=Associated%20with%20th.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 А. П. Малецький, О. В. Хомякова

This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International (CC BY 4.0) that allows users to read, download, copy, distribute, print, search, or link to the full texts of the articles, or use them for any other lawful purpose, without asking prior permission from the publisher or the author as long as they cite the source.
COPYRIGHT NOTICE
Authors who publish in this journal agree to the following terms:
- Authors hold copyright immediately after publication of their works and retain publishing rights without any restrictions.
- The copyright commencement date complies the publication date of the issue, where the article is included in.
DEPOSIT POLICY
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) during the editorial process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work with an acknowledgement of its initial publication in this journal.
- Post-print (post-refereeing manuscript version) and publisher's PDF-version self-archiving is allowed.
- Archiving the pre-print (pre-refereeing manuscript version) not allowed.