Papilledema in chronic subdural hematoma: how often it is seen and what has changed?
DOI:
https://doi.org/10.31288/oftalmolzh202235862Keywords:
chronic subdural hematoma, diagnostic assessment, papilledema, optic nerve, headache, ageAbstract
Background: A chronic subdural hematoma (CSDH) is defined as an encapsulated accumulation of a clot of blood and degraded blood products on the surface of the brain between the dural and arachnoid membranes. Papilledema had for a long time been referred to as a characteristic objective symptom of CSDH. The incidence of papilledema is however, variable and depends on a variety of factors.
Purpose: To analyze the data on the diagnosis of papilledema in patients with CSDH and to review the place of papilledema among the clinical findings in CSDH.
Material and Methods: We retrospectively reviewed the medical records of 164 patients with CSDH who underwent treatment at the Romodanov Neurosurgery Institute and Zaporizhzhia City Clinical Emergency Care Hospital from 2011 through 2021. Patients underwent clinical-and-neurological, ophthalmological, and neuroimaging examinations.
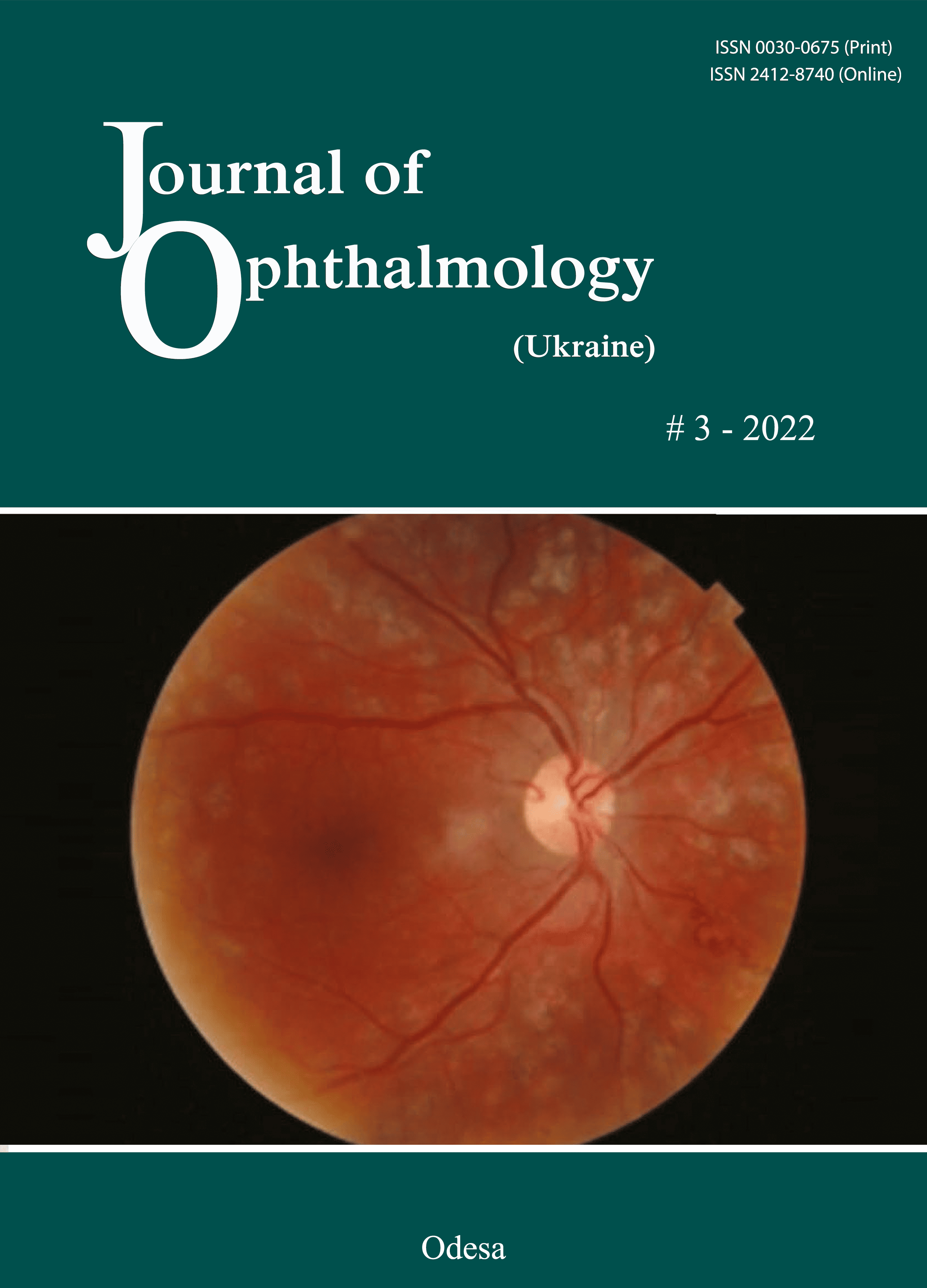
Results: Papilledema was found in 4 (2.4%) of the patients. All these four patients had moderate papilledema which regressed after surgery. Details of these cases were reviewed.
Conclusion: A shift in the peak incidence of CSDH towards an older age group and an increasing use of neuroimaging modalities exert an impact on the incidence of papilledema in patients with CSDH. Papilledema was found in 2.4% of the patients of the study.
References
1.Feghali J, Yang W, Huang J. Updates in Chronic Subdural Hematoma: Epidemiology, Etiology, Pathogenesis, Treatment, and Outcome. World Neurosurg. 2020 Sep;141:339-345. https://doi.org/10.1016/j.wneu.2020.06.140
2.Bartek J Jr, Sjavik K, Stahl F, Kristiansson H, Solheim O, Gulati S, et al. Surgery for chronic subdural hematoma in nonagenarians: a Scandinavian population-based multicenter study. Acta Neurol Scand. 2017 Nov;136(5):516-20. https://doi.org/10.1111/ane.12764
3.Ou Y, Dong J, Wu L, Xu L, Wang L, Liu B, et al. A comparative study of chronic subdural hematoma in three age ranges: Below 40 years, 41-79 years, and 80 years and older. Clin Neurol Neurosurg. 2019 Mar;178:63-69. https://doi.org/10.1016/j.clineuro.2019.01.018
4.Balser D, Farooq S, Mehmood T, Reyes M, Samadani U. Actual and projected incidence rates for chronic subdural hematomas in United States Veterans Administration and civilian populations. J Neurosurg. 2015 Nov; 123(4):1209-15. https://doi.org/10.3171/2014.9.JNS141550
5.Eliseeva NM, Serova NK. [Papilledema and its differential diagnosis: A guide for physicians]. Moscow: Triadа; 2018. Russian.
6.Scott СJ, Kardon RH, Lee AG, Frissen L. Diagnosis and grading of papilledema in patient with raised intracranial pressure using optical coherence tomography vs clinical experts assessment using a clinical staging scale. Arch Ophthalmol. 2010;128(6):705-11. https://doi.org/10.1001/archophthalmol.2010.94
7.Mohamed MT, Aldghamy AH, Elsoghair OA. Diagnosis and grading of papilledema using optical coherence tomography compared to clinical staging by Frise'n Scale. SVU-IJMS. 3(2):14-19. https://doi.org/10.21608/svuijm.2020.111890
8.Greenberg D, Aminoff M, Simon R, eds. Lange Clinical Neurology. 11th edition. New York, NY: McGraw-Hill Education; 2020.
9.Liu GT, Volpe NJ, Galetta SL, eds. Neuro-ophthalmology: Diagnosis and Management. 3rd edition. London: Elsevier Saunders; 2018.
10.Advances in Neurotraumatology. Vigouroux RP, Editor-in-Chief. Volume 1. Extracerebral Collections. McLaurin RL, Managing Editor. Wien: Springer-Verlag; 1986.
11.Handbook of ophthalmologic emergencies: a guide for emergencies in ophthalmology. Gombos GM, edr. Flushing, NY: Medical Examination Pub.; 1973.
12.Zasler ND, Katz DI, Zafonte RD, eds. Brain injury medicine: principles and practice. 2nd ed. New York, NY: Demos Medical Publishing; 2012. https://doi.org/10.1891/9781617050572
13.Mahapatra AK, Kamal R, Kumar R, eds. Textbook of Traumatic Brain Injury. New Delhi, India: Jaypee Brothers Medical Publishers; 2012. https://doi.org/10.5005/jp/books/11654_6
14.Kuddus R, Hossain MA, Hossain SKS, Hossain ATMM, Debnath H, Rahman A, et al. Study on clinical features and factors associated with thickness of chronic subdural hematoma in adult. Bangabandhu Sheikh Mujib Med Univ J. 2018; 11: 209-12. https://doi.org/10.3329/bsmmuj.v11i3.37701
15.Yamada SM, Teramoto A, Yamada S, Hoshiai YC. Severe papilledema identified 3 weeks after head injury. Neurol Med Chir (Tokyo). 2002 Jul;42(7):293-6. https://doi.org/10.2176/nmc.42.293
16.Park SH, Kim YS, Chung SS, Lee KC. Clinical Analysis of Treatment of Chronic Subdural Hematoma. J Korean Neurosurg Soc. 1984 Dec; 13(4): 669-79.
17.Yamada SM, Tomita Y, Murakami H, Nakane M, Yamada S, Murakami M, et al. Headache in patients with chronic subdural hematoma: analysis in 1080 patients. Neurosurg Rev. 2018 Apr;41(2):549-56. https://doi.org/10.1007/s10143-017-0889-x
18.Bartek J, Sjåvik K, Dhawan S, Sagberg LM, Kristiansson H, Ståhl F, et al. Clinical Course in Chronic Subdural Hematoma Patients Aged 18-49 Compared to Patients 50 Years and Above: A Multicenter Study and Meta-Analysis. Front Neurol. 2019 Apr 5;10:311. https://doi.org/10.3389/fneur.2019.00311
19.Wang HS, Kim SW, Kim SH. Spontaneous chronic subdural hematoma in an adolescent girl. J Korean Neurosurg Soc. 2013 Mar; 53(3):201-3. https://doi.org/10.3340/jkns.2013.53.3.201
20.Emamhadi M, Chabok SY, Alijani B, Behzadnia H, Rasoulian J, Andalib S. Spontaneous Chronic Subdural Hematoma: A Case Report and Literature Review. Trauma Mon. 2017 November; 22(6):e38529. https://doi.org/10.5812/traumamon.38529
21.Dulani S, Dulani R, Lele S, Diagavane S, Anjankar S, Jaiswal N, et al. Chronic Subdural Haematoma in a Case of Hyperthyroidism Presenting with Papilledema. Chinese Medicine. 2012; 3 (4):179-81. https://doi.org/10.4236/cm.2012.34027
22.Won YD, Yi HJ, Lee YJ, Chun HJ, Cho H, Bak KH. Chronic Subdural Hematoma in Young Adult: An Age Comparison Study. Korean J Neurotrauma. 2013;9:6-11. https://doi.org/10.13004/kjnt.2013.9.1.6
23.Kaste M, Waltimo O, Heiskanen O. Chronic bilateral subdural haematoma in adults. Acta Neurochir (Wien). 1979;48(3-4):231-6. https://doi.org/10.1007/BF02056971
24.Ou Y, Yu X, Liu X, Jing Q, Liu B, Liu W. A Comparative Study of Chronic Subdural Hematoma in Patients With and Without Head Trauma: A Retrospective Cross Sectional Study. Front Neurol. 2020 Nov 27;11:588242. https://doi.org/10.3389/fneur.2020.588242
25.Iantosca MR, Simon RH. Chronic subdural hematoma in adult and elderly patients. Neurosurg Clin N Am. 2000 Jul;11(3):447-54. https://doi.org/10.1016/S1042-3680(18)30107-4
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 М. В. Каджая, Т. А. Малишева, В. А. Васюта, О. С. Готін, А. О. Дядечко, Л. Р. Боровік

This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International (CC BY 4.0) that allows users to read, download, copy, distribute, print, search, or link to the full texts of the articles, or use them for any other lawful purpose, without asking prior permission from the publisher or the author as long as they cite the source.
COPYRIGHT NOTICE
Authors who publish in this journal agree to the following terms:
- Authors hold copyright immediately after publication of their works and retain publishing rights without any restrictions.
- The copyright commencement date complies the publication date of the issue, where the article is included in.
DEPOSIT POLICY
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) during the editorial process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work with an acknowledgement of its initial publication in this journal.
- Post-print (post-refereeing manuscript version) and publisher's PDF-version self-archiving is allowed.
- Archiving the pre-print (pre-refereeing manuscript version) not allowed.