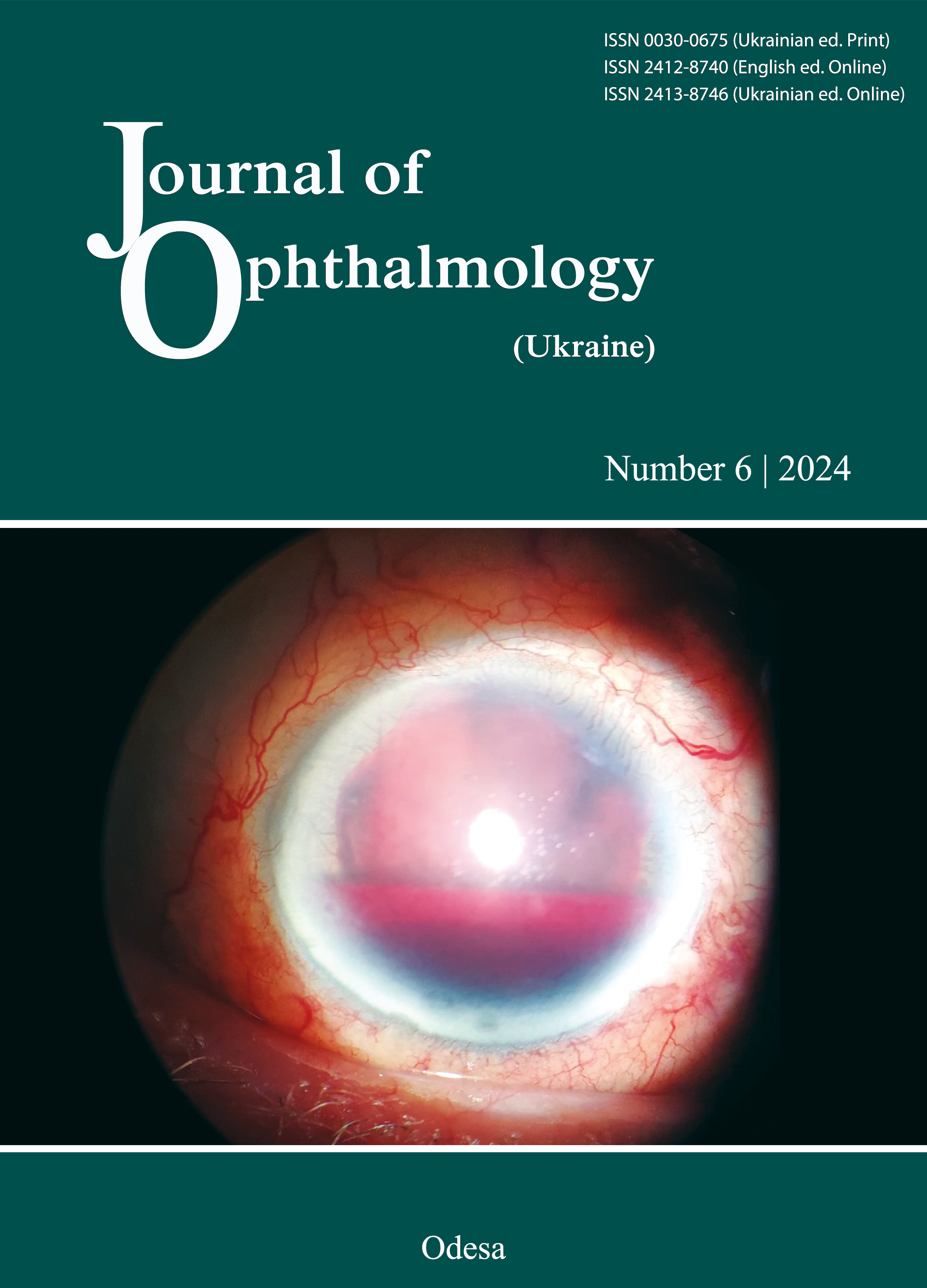
Features of the course of post-COVID-19 primary and recurrent herpetic keratitis
DOI:
https://doi.org/10.31288/oftalmolzh2024639Keywords:
COVID 19, herpetic keratitis, recurrent herpetic keratitis, herpes simplex virus, corneal traumaAbstract
Purpose: To assess the features of the course of post-COVID-19 primary and recurrent herpetic keratitis (HK).
Material and Methods: Medical records of 70 patients (83 eyes) with post-COVID-19 HK were reviewed. The patients were divided into two groups: group 1 with primary HK (26 patients; 30 eyes) and group 2 with recurrent HK (44 patients; 53 eyes). COVID-19 severity was defined as mild (without evidence of viral pneumonia), moderate (pneumonia not treated at the intensive care unit (ICU)) and severe (treatment at the ICU). Levels of total vitamin D, and immunoglobulin G (IgG) against the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike protein, herpes simplex virus (HSV)-1/2, cytomegalovirus (CMV) and Epstein-Barr nuclear antigen (EBNA) in venous blood were assessed.
Results: Dendritic HK and ulcerative necrotizing HK were more common in patients with primary keratitis than in recurrent keratitis (20.7% vs 2% and 41.2% vs 15.6%, respectively). Non-necrotizing stromal HK was more common in the latter patients than in the former patients (82.4% vs 37.9%, respectively) and was the most common form of post-COVID-19 HK in both groups. Ulcerative necrotizing HK was more common in patients with primary HK than in patients with recurrent HK (41.4% vs 15.6%, respectively) and was mainly observed after severe COVID-19. In patients with ulcerative necrotizing HK, the level of HSV IgG was 1.6 times higher than in patients with epithelial HK, and 1.5 times higher than in patients with non-necrotizing stromal HK. Elevated anti-VZV, anti-EBNA, and anti-CMV IgG levels were found in 93.2%, 76.4%, and 86.4%, respectively, of the examined patients.
Conclusion: SARS CoV 2 infection may be a potential risk factor for HSV reactivation from latency and primary or recurrent HK, with an increase in the frequency of bilateral ocular lesions and stromal forms of HK. The ophthalmologist must be aware of this ocular complication in COVID 19–infected cases, which may present either during acute or recovery phase of the illness; it mostly occurs in severely infected patients.
References
Velavan ThP, Meyer ChG. The COVID-19 epidemic. Trop Med Int Health. 2020 Mar;25(3):278-280. doi: 10.1111/tmi.13383. Epub 2020 Feb 16. https://doi.org/10.1111/tmi.13383
Ahmad B, Gurnani B , Patel BC. Herpes Simplex Keratitis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan.2024 Mar 10.
St. Leger AJ, Rowe AM, Jeon S. et al. Herpes keratitis. Progress in retinal & eye research. 2013;13: 88-101. https://doi.org/10.1016/j.preteyeres.2012.08.002
Sanjay S, Srinivasan P, Jayadev C, Mahendradas P, Gupta A, Kawali A, et al. Post COVID-19 ophthalmic manifestations in an Asian Indian male. Ocul Immunol Inflamm. 2021;29:656-61. https://doi.org/10.1080/09273948.2020.1870147
Sanjay S, Rao VK, Mutalik D, Mahendradas P, Kawali A, Shetty R. Post coronavirus disease 19: Hyper inflammatory syndrome associated bilateral anterior uveitis and multifocal serous retinopathy secondary to steroids. Indian J Rheumatol. 2021;16:451-5. https://doi.org/10.4103/injr.injr_330_20
Sanjay S, Singh YP, Roy D, Mahendradas P, Kawali A, Shetty R. Recurrent bilateral idiopathic anterior uveitis with vitritis post coronavirus disease 2019 infection. Indian J Rheumatol. 2021;16:460-3. https://doi.org/10.4103/injr.injr_114_21
Sanjay S, Mutalik D, Gowda S, Mahendradas P, Kawali A, Shetty R. Post Coronavirus disease (COVID-19) reactivation of a quiescent unilateral anterior uveitis. SN ComprClin Med. 2021;3:1843-7. https://doi.org/10.1007/s42399-021-00985-2
Sanjay S, Gowda PB, Rao B, Mutalik D, Mahendradas P, Kawali A, et al. «Old wine in a new bottle» - post COVID-19 infection, central serous chorioretinopathy and the steroids. J Ophthalmic Inflamm Infect. 2021;11:14. https://doi.org/10.1186/s12348-021-00244-4
Mahendradas P, Hande P, Patil A, Kawali A, Sanjay S, Ahmed SA, et al. Bilateral post fever retinitis with retinal vascular occlusions following severe acute respiratory syndrome corona virus (SARS-CoV2) infection. Ocul Immunol Inflamm. 2022;30:1715-20. https://doi.org/10.1080/09273948.2021.1936564
Sanjay S, Kawali A, Agrawal S, Mahendradas P. Unilateral acute anterior sclero-uveitis preceding Corona virus disease (COVID-19) Pan Am J Ophthalmol. 2022;4:26. https://doi.org/10.4103/pajo.pajo_14_22
Puri P, Parnami P, Athwal PSS, Kumari S, Kumar C, Suri Y. COVID-19 Rekindling Herpes Zoster in an immunocompetent patient. Cureus. 2021;13:e18049. https://doi.org/10.7759/cureus.18049
Pourazizi M, Dehghani S, Abtahi-Naeini B. Herpes zoster oftálmico y COVID-19: ¿Complicación post-COVID-19 o coincidencia? [Herpes Zoster Ophthalmicus and COVID-19:A Post-COVID-19 Complication or a Coincidence? Actas Dermosifiliogr. 2022;113:S16-S17. Spanish. https://doi.org/10.1016/j.ad.2021.10.001
Cano-Ortiz A, Leiva-Gea I, Ventosa ÁS,et al. Stromal interstitial keratitis in a patient with COVID-19.J Fr Ophtalmol. 2022 Apr; 45(4): e175-e177. https://doi.org/10.1016/j.jfo.2021.11.004
World Health Organization. COVID-19 clinical management: living guidance, 25 January 2021. Access: https://iris.who.int/handle/10665/338882. License: CC BY-NC-SA 3.0 IGO.
Liesegang TJ. Classification of Herpes Simplex Virus Keratitis and Anterior Uveitis. Cornea, 1999, 18, 127-143 https://doi.org/10.1097/00003226-199903000-00001
Li H, Zhang J, Kumar A, Zheng M, Atherton SS, Yu FS Herpes simplex virus 1 infection induces the expression of proinflammatory cytokines, interferons and TLR7 in human corneal epithelial cells. Immunology. 2006 Feb;117(2):167-76. https://doi.org/10.1111/j.1365-2567.2005.02275.x
Yildiz BK, Ozkan D, Tellioglu A, Demirok A. Is COVID-19 Infection a Trigger for Herpetic Stromal Keratitis? Beyoglu Eye J. 2022 May 27;7(2):140-142.
Musa M, Enaholo E, Aluyi-Osa G, Atuanya GN, Spadea L, Salati C, Zeppieri M. Herpes simplex keratitis: A brief clinical overview. World J Virol. 2024 Mar 25;13(1):89934. https://doi.org/10.5501/wjv.v13.i1.89934
Le Balc'h P, Pinceaux K, Pronier C, Seguin P, Tadie J-M, Reizine F Herpes simplex virus and cytomegalovirus reactivations among severe COVID-19 patients. Crit Care 2020 Aug 28;24(1):530. https://doi.org/10.1186/s13054-020-03252-3
Seeßle J, Hippchen T, Schnitzler P, Gsenger J, Giese T, Merle U High rate of HSV-1 reactivation in invasively ventilated COVID- 19 patients: Immunological findings. PLoS One. 2021 Jul 1;16(7):e0254129. https://doi.org/10.1371/journal.pone.0254129
Hernandez JM, Singam H, Babu A, Aslam S, Lakshmi S SARS-CoV-2 infection (COVID-19) and herpes simplex virus-1 conjunctivitis: Concurrent viral infections or a cause-effect result? Cureus. 2021 Jan; 13(1): e12592. https://doi.org/10.7759/cureus.12592
Majtanova N, Kriskova P, Keri P, Fellner Z, Majtan J, Kolar P Herpes simplex keratitis in patients with SARS-CoV-2 infection: A series of five cases. Medicina 2021; 57(5): 412. https://doi.org/10.3390/medicina57050412
Lobo AM, Agelidis AM, Shukla D. Pathogenesis of herpes simplex keratitis: The host cell response and ocular surface sequelae to infection and inflammation. Ocul Surf. 2019 Jan;17(1):40-49. https://doi.org/10.1016/j.jtos.2018.10.002
Chaloulis SK, Mousteris G, Tsaousis KT. Incidence and Risk Factors of Bilateral Herpetic Keratitis: 2022 Update. Trop Med Infect Dis. 2022 Jun 7;7(6):92. https://doi.org/10.3390/tropicalmed7060092
Hashido M, Kawana T. Herpes simplex virus-specific IgM, IgA and IgG subclass antibody responses in primary and nonprimary genital herpes patients. Microbiol Immunol. 1997;41(5):415-20. https://doi.org/10.1111/j.1348-0421.1997.tb01872.x
Meng M, Zhang S, Dong X, Sun W, Deng Y, Li W, et al. COVID-19 associated EBV reactivation and effects of ganciclovir treatment. Immun Inflamm Dis. 2022 Apr;10(4):e597. https://doi.org/10.1002/iid3.597
Su Y, Yuan D, Chen DG, Ng RH, Wang K, Choi J, et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell. 2022; 185 :881-895.e20. https://doi.org/10.1016/j.cell.2022.01.014
Sridharan M, Navitskas SD, Kock EM, Houghton DE, Heikal NM, Chen D, Pruthi KR. Evaluation of soluble fibrin monomer complex in patients in SARS-CoV-2 COVID-19 infection-associated coagulopathy. Eur J Haematol. 2022 Apr;108(4):319-326. Epub 2022 Jan 10. https://doi.org/10.1111/ejh.13738
Bouillon R, Marcocci C, Carmeliet G, Bikle D, White JH, Dawson-Hughes B, et al. Skeletal and Extraskeletal Actions of Vitamin D: Current Evidence and Outstanding Questions. Endocr Rev. 2019 Aug 1;40(4):1109-1151. https://doi.org/10.1210/er.2018-00126
Domazet Bugarin J, Dosenovic S, Ilic D, Delic N, Saric I, Ugrina I, et al. Vitamin D Supplementation and Clinical Outcomes in Severe COVID-19 Patients-Randomized Controlled Trial. Nutrients. 2023 Feb 28;15(5):1234. https://doi.org/10.3390/nu15051234
Das N, Das J, Pal D.Stromal and endothelial herpes simplex virus keratitis reactivation in the convalescent period of COVID-19 - A case report. Indian J Ophthalmol. 2022 Mar 22;70(4):1410-1412. https://doi.org/10.4103/ijo.IJO_2838_21
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Drozhzhyna G. I., Sereda K. V., Khramenko N. I.,

This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International (CC BY 4.0) that allows users to read, download, copy, distribute, print, search, or link to the full texts of the articles, or use them for any other lawful purpose, without asking prior permission from the publisher or the author as long as they cite the source.
COPYRIGHT NOTICE
Authors who publish in this journal agree to the following terms:
- Authors hold copyright immediately after publication of their works and retain publishing rights without any restrictions.
- The copyright commencement date complies the publication date of the issue, where the article is included in.
DEPOSIT POLICY
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) during the editorial process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work with an acknowledgement of its initial publication in this journal.
- Post-print (post-refereeing manuscript version) and publisher's PDF-version self-archiving is allowed.
- Archiving the pre-print (pre-refereeing manuscript version) not allowed.