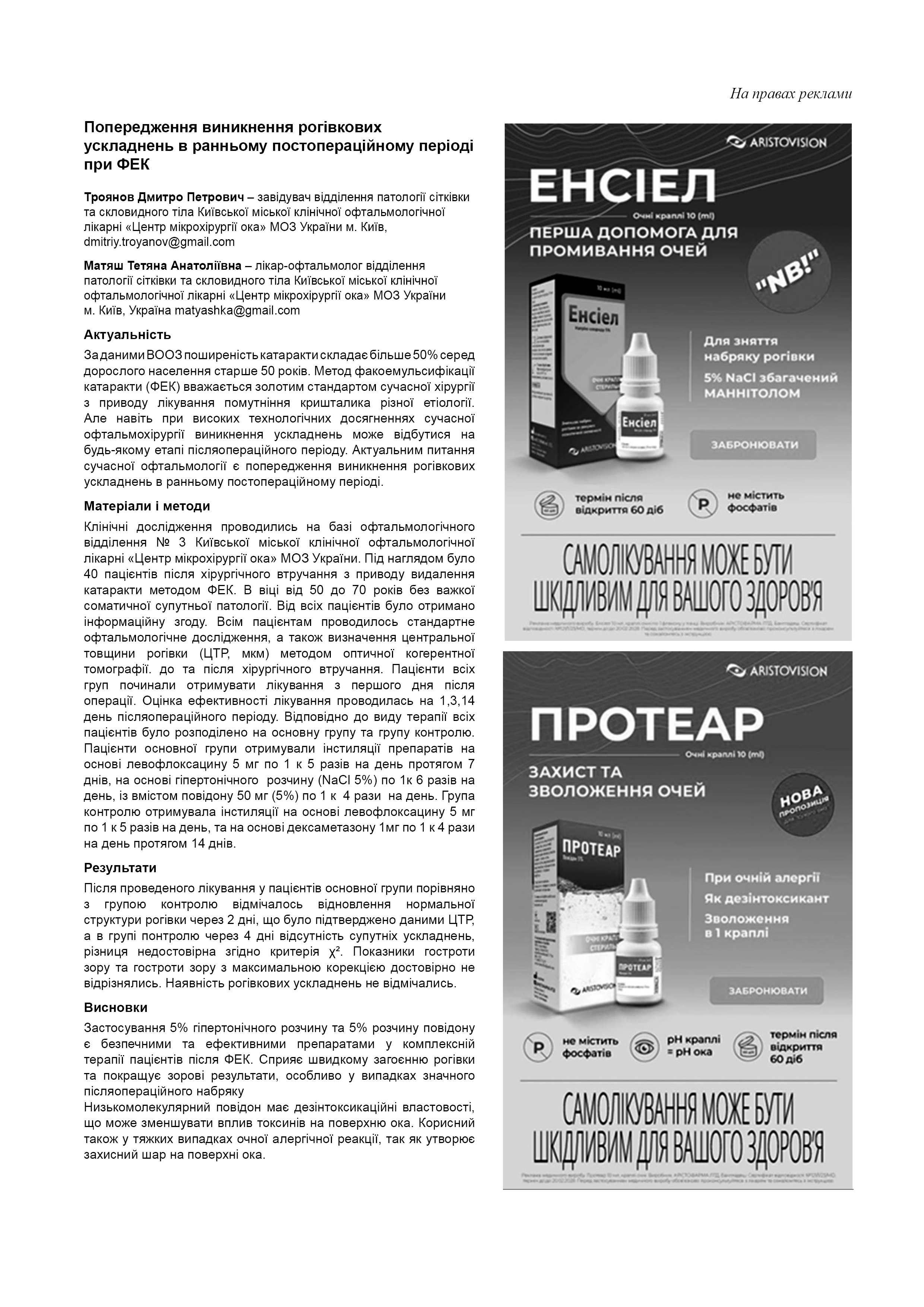
Regional hemodynamics of the eye in optic neuritis
DOI:
https://doi.org/10.31288/oftalmolzh20232310Abstract
Background: Optic nerve disease accounts for up to 28% of all cases of visual disability. Although recent studies have demonstrated abnormal hemodynamics in optic neuritis (ON), results of different studies as well as data on the pathophysiology of vascular abnormalities are contradictory.
Purpose: To assess regional hemodynamics on the basis of ophthalmic rheography (ORG) and rheoencephalography (REG) in patients with optic neuritis and those with complications of the disease.
Material and Methods: Fifty-seven patients (82 affected eyes; 27 women and 30 men) who were examined for idiopathic ON at the Department of Ocular Inflammatory Disease, Filatov Institute of Eye Disease and Tissue Therapy, were included in the study and divided into four groups. They underwent a clinical ophthalmological examination as well as ORG and REG studies with the computerized rheography apparatus Reocom (Kharkiv).
Results: Best-corrected visual acuity (BCVA) values were twofold to threefold lower for the eyes with partial optic atrophy (POA) after ON or those with macular involvement in ON than for the eyes with acute ON or prolonged ON. BCVA showed mild direct correlation with ocular pulse blood filling (OPBF) expressed as RQ (r = 0.24; р < 0.05), and negative correlation with the presence of complications following ON (r = -0.35; р < 0.05). RQ values in patients with acute ON were 15.5% higher than in controls (р < 0.05) and 35% and 31% higher than in patients with POA following ON and patients developing macular lesion following ON, respectively (р < 0.05). RQ values in patients with partial optic atrophy (POA) were 23.6% lower than in controls (р < 0.05), which reflected regional ischemic process. The odds ratio (OR) for the presence of a reduced RQ value (a) in the eye with POA following ON compared to the eye with acute ON was 9.2 (P < 0.05, 95% confidence interval 2.0–42.4), and (b) in the eye developing macular lesion following ON compared to the eye with acute ON was 4.3 (P < 0.05, 95% CI, 1.2–14.7). Pulse blood filling as assessed by rheography index (RI) in the internal carotid artery (ICS) was actually normal in patients with acute ON and 44% increased in patients with prolonged ON or outcome of ON compared to controls (р < 0.05). In addition, tonicity of large vessels in the ICS and VBS as assessed by alpha/Т (%) was normal in patients with acute ON and at average 15% higher in patients with complications following ON. Moreover, tonicity of small-caliber vessels as assessed by the dicrotic index (DCI) and diastolic index (DSI) values was at average 32.2% and 55%, respectively, higher in patients than in controls.
Conclusion: We revealed features of ocular and brain hemodynamics in patients with acute ON, prolonged ON and those with complications of the disease.
References
Палько В. Ефективність комбінованого лікування Beck RW, Cleary PA, Anderson MM Jr, Keltner JL, Shults WT, Kaufman DI, Buckley EG, et al. A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis. The Optic Neuritis Study Group. N Engl J Med. 1992 Feb 27;326(9):581-8. https://doi.org/10.1056/NEJM199202273260901
Hickman SJ, Petzold A. Update on Optic Neuritis: An International View. Neuroophthalmology. 2021 Aug 31;46(1):1-18. https://doi.org/10.1080/01658107.2021.1964541
Bennett JL. Optic Neuritis. Continuum (Minneap Minn). 2019 Oct;25(5):1236-64. https://doi.org/10.1212/CON.0000000000000768
Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, et al. International Panel for NMO Diagnosis. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015 Jul 14;85(2):177-89. https://doi.org/10.1212/WNL.0000000000001729
Pache M, Kaiser HJ, Akhalbedashvili N, Lienert C, Dubler B, Kappos L, et al. Extraocular blood flow and endothelin-1 plasma levels in patients with multiple sclerosis. Eur Neurol. 2003;49(3):164-8. https://doi.org/10.1159/000069085
Hradílek P, Zapletalova O, Dolezil D, Skoloudik D. Acute optic neuritis in multiple sclerosis: evaluation of haemodynamics in the ophthalmic artery with colour Doppler imaging. Neuroophthalmology. 2005;29:161-4. https://doi.org/10.1080/01658100500218012
McLeod D, Marshall J, Kohner EM. Role of axoplasmic transport in the pathophysiology of ischaemic disc swelling. Br J Ophthalmol. 1980 Apr;64(4):247-61. https://doi.org/10.1136/bjo.64.4.247
Lightman S, McDonald WI, Bird AC, Francis DA, Hoskins A, Batchelor JR, et al. Retinal venous sheathing in optic neuritis. Its significance for the pathogenesis of multiple sclerosis. Brain. 1987 Apr;110 (Pt 2):405-14. https://doi.org/10.1093/brain/110.2.405
Lee TH, Ji YS, Park SW, Heo H. Retinal ganglion cell and axonal loss in optic neuritis: risk factors and visual functions. Eye (Lond). 2017 Mar;31(3):467-474. https://doi.org/10.1038/eye.2016.253
Храменко НИ, Коновалова НВ. Состояние гемодинамики глаза при неврите зрительного нерва. Мат. науково-практич. конф. з міжнар. участю Філатовські читання-2019; 2019 травня 23-24; Одеса. Одеса; 2019, с. 127.
Храменко НИ, Коновалова НВ, Величко ЛН, Богданова АВ. Особенности иммунологического статуса у больных при неврите зрительного нерва. . Матер. науково-практич. конф. з міжнар. участю Філатовські читання-2019; 2019 травня 23-24; Одеса. Одеса; 2019, с. 126.
Jonzzon S, Suleiman L, Yousef A, Young B, Hart J, Peschl P, et al. Clinical Features and Outcomes of Pediatric Monophasic and Recurrent Idiopathic Optic Neuritis. J Child Neurol. 2020 Jan;35(1):77-83. https://doi.org/10.1177/0883073819877334
Balcer LJ. Clinical practice. Optic neuritis. N Engl J Med. 2006 Mar 23;354(12):1273-80. https://doi.org/10.1056/NEJMcp053247
Foroozan R, Buono LM, Savino PJ, Sergott RC. Acute demyelinating optic neuritis. Curr Opin Ophthalmol. 2002 Dec;13(6):375-80. https://doi.org/10.1097/00055735-200212000-00006
Karami M, Janghorbani M, Dehghani A, Riahinejad M. Orbital Doppler evaluation of blood flow velocities in optic neuritis. Korean J Ophthalmol. 2012 Apr;26(2):116-22. https://doi.org/10.3341/kjo.2012.26.2.116
Henderson AP, Altmann DR, Trip AS, Kallis C, Jones SJ, Schlottmann PG, et al. A serial study of retinal changes following optic neuritis with sample size estimates for acute neuroprotection trials. Brain. 2010 Sep;133(9):2592-602. https://doi.org/10.1093/brain/awq146
Beck RW, Gal RL, Bhatti MT, Brodsky MC, Buckley EG, Chrousos GA, et al. Optic Neuritis Study Group. Visual function more than 10 years after optic neuritis: experience of the optic neuritis treatment trial. Am J Ophthalmol. 2004 Jan;137(1):77-83. https://doi.org/10.1016/S0002-9394(03)00862-6
Optic Neuritis Study Group. Visual function 15 years after optic neuritis: a final follow-up report from the Optic Neuritis Treatment Trial. Ophthalmology. 2008 Jun;115(6):1079-82.e5. https://doi.org/10.1016/j.ophtha.2007.08.004
Miller NR, Newman NJ, Biousse V, Kerrison JB. Walsh and Hoyt's Clinical Neuro-ophthalmology. Lippincott Williams & Wilkins: Philadelphia, PA;2005.320 p.
Trip SA, Schlottmann PG, Jones SJ, Altmann DR, Garway-Heath DF, Thompson AJ, et al. Retinal nerve fiber layer axonal loss and visual dysfunction in optic neuritis. Ann Neurol. 2005 Sep;58(3):383-91. https://doi.org/10.1002/ana.20575
Costello F, Coupland S, Hodge W, Lorello GR, Koroluk J, Pan YI, et al. Quantifying axonal loss after optic neuritis with optical coherence tomography. Ann Neurol. 2006 Jun;59(6):963-9. https://doi.org/10.1002/ana.20851
Burkholder BM, Osborne B, Loguidice MJ, Bisker E, Frohman TC, Conger A, et al. Macular volume determined by optical coherence tomography as a measure of neuronal loss in multiple sclerosis. Arch Neurol. 2009 Nov;66(11):1366-72. https://doi.org/10.1001/archneurol.2009.230
Walter SD, Ishikawa H, Galetta KM, Sakai RE, Feller DJ, Henderson SB, et al. Ganglion cell loss in relation to visual disability in multiple sclerosis. Ophthalmology. 2012 Jun;119(6):1250-7. https://doi.org/10.1016/j.ophtha.2011.11.032
Viturino MGM, Moura FC. Recurrent idiopathic neuroretinitis as a spectrum of atypical optic neuritis: a case report and literature review. Arq Bras Oftalmol. 2018 Jan-Feb;81(1):70-2. https://doi.org/10.5935/0004-2749.20180016
Acevedo AR, Nava C, Arriada N, Violante A, Corona T. Cardiovascular dysfunction in multiple sclerosis. Acta Neurol Scand. 2000 Feb;101(2):85-8. https://doi.org/10.1034/j.1600-0404.2000.101002085.x
Karaali K, Senol U, Aydin H, Cevikol C, Apaydin A, Lüleci E. Optic neuritis: evaluation with orbital Doppler sonography. Radiology. 2003 Feb;226(2):355-8. https://doi.org/10.1148/radiol.2262011915
Akarsu C, Tan FU, Kendi T. Color Doppler imaging in optic neuritis with multiple sclerosis. Graefes Arch Clin Exp Ophthalmol. 2004 Dec;242(12):990-4. https://doi.org/10.1007/s00417-004-0948-1
Modrzejewska M, Karczewicz D, Wilk G. Assessment of blood flow velocity in eyeball arteries in multiple sclerosis patients with past retrobulbar optic neuritis in color Doppler ultrasonography. Klin Oczna. 2007;109(4-6):183-6.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Наталя Храменко, Наталія Коновалова , Тетяна Серебріна, Олена Іваницька

This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International (CC BY 4.0) that allows users to read, download, copy, distribute, print, search, or link to the full texts of the articles, or use them for any other lawful purpose, without asking prior permission from the publisher or the author as long as they cite the source.
COPYRIGHT NOTICE
Authors who publish in this journal agree to the following terms:
- Authors hold copyright immediately after publication of their works and retain publishing rights without any restrictions.
- The copyright commencement date complies the publication date of the issue, where the article is included in.
DEPOSIT POLICY
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) during the editorial process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work with an acknowledgement of its initial publication in this journal.
- Post-print (post-refereeing manuscript version) and publisher's PDF-version self-archiving is allowed.
- Archiving the pre-print (pre-refereeing manuscript version) not allowed.

.png)