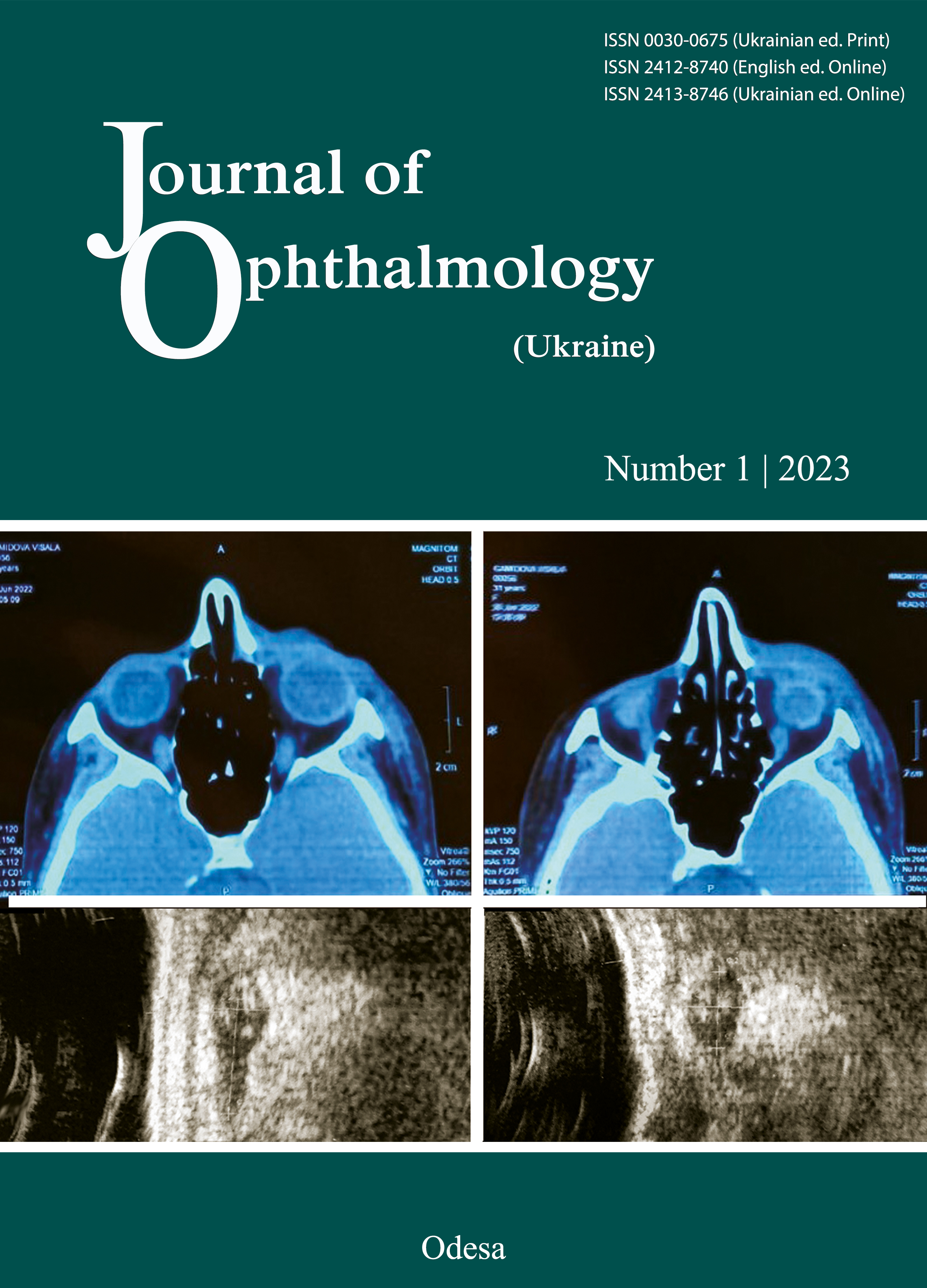
Periocular basal cell carcinoma of the eyelids – review
DOI:
https://doi.org/10.31288/oftalmolzh202316767Ключові слова:
periocular tumours, nonmelanoma skin cancer, basal cell carcinoma, Mohs surgery, vismodegibАнотація
Introduction. Basal cell carcinoma is the most common tumour of the eyelids and periocular region throughout the world. BCC represents 90 % of malignant tumours of the eyelids, predominantly in the male population. The incidence is higher in age over 60. Over 50% of BCC of the periocular region initially occur on the lower lid and inner angle.
Research objectives. Literature review of the epidemiology, aetiopathogenesis, clinical attributes, diagnostics, treatment histopathology, recurrence, prognostic factors, and management of BCC.
Core of work. Standardised incidence of diagnosis C44 in the period 1997–2012 in Slovakia ranged from 35.05 to 73.9 cases per 100,000 inhabitants. The histopathological examination is essential. The first consideration for treatment of periocular BCC is radical surgical excision using Mohs micrographic technique. We can consider the apoptotic index, the expression of Bcl-2, as an unexplained prognostic factor of BCC recurrence.
Conclusion. Increased attention must be given to periocular malignant tumours. Functional and aesthetic outcome in patients is important after clear excisions and reconstruction should be carefully considered. Radical exenteration is considered in the case of orbital invasion of high-risk aggressive BCC.
Посилання
Prídavková Z, Bieliková A, Ferková N, Lysková D. Recurrent periocular basal cell carcinoma. Case report. Cesk Slov Oftalmol. 2021 Spring;77(4):208-213. https://doi.org/10.31348/2021/24
Saleh GM, Desai P, Collin JRO, Ives A, et al. Incidence of eyelid basal cell carcinoma in England: 2000-2010. Br J Ophthalmol. 2017;101(2):209-12. https://doi.org/10.1136/bjophthalmol-2015-308261
Sun MT, Wu A, Figueira E, et al. Management of periorbital basal cell carcinoma with orbital invasion. Future Oncol Lond Engl. 2015 Nov;11(22):3003-10. https://doi.org/10.2217/fon.15.190
Furdova A, Kapitanova K, Kollarova A, Sekac J. Periocular basal cell carcinoma - clinical perspectives. Oncol Rev. 2020 Apr 30;14(1):420. https://doi.org/10.4081/oncol.2020.420
Madge SN, Khine AA, Thaller VT, Davis G, et al. Globe-sparing surgery for medial canthal Basal cell carcinoma with anterior orbital invasion. Ophthalmology. 2010 Nov;117(11):2222-8. https://doi.org/10.1016/j.ophtha.2010.02.013
Sun MT, Wu A, Huilgol SC, Selva D. Accuracy of Biopsy in Subtyping Periocular Basal Cell Carcinoma. Ophthal Plast Reconstr Surg. 2015 Dec;31(6):449-51. https://doi.org/10.1097/IOP.0000000000000372
Leibovitch I, McNab A, Sullivan T, et al. Orbital invasion by periocular basal cell carcinoma. Ophthalmology. 2005 Apr;112(4):717-23. https://doi.org/10.1016/j.ophtha.2004.11.036
Shields JA, Shields CL, Demirci H, et al. Experience with eyelid-sparing orbital exenteration: the 2000 Tullos O. Coston Lecture. Ophthal Plast Reconstr Surg. 2001 Sep;17(5):355-61. https://doi.org/10.1097/00002341-200109000-00010
Ben Simon GJ, Schwarcz RM, Douglas R, et al. Orbital exenteration: one size does not fit all. Am J Ophthalmol. 2005 Jan;139(1):11-7. https://doi.org/10.1016/j.ajo.2004.07.041
Furdova A, Lukacko P. Periocular Basal Cell Carcinoma Predictors for Recurrence and Infiltration of the Orbit. J Craniofac Surg. 2017 Jan;28(1):e84-7. https://doi.org/10.1097/SCS.0000000000003242
Wehner MR, Linos E, Parvataneni R, et al. Timing of subsequent new tumors in patients who present with basal cell carcinoma or cutaneous squamous cell carcinoma. JAMA Dermatol. 2015 Apr;151(4):382-8. https://doi.org/10.1001/jamadermatol.2014.3307
Ding S, Sagiv O, Guo Y, et al. Change in Eyelid Carcinoma T Category With Use of the 8th Versus 7th Edition of the American Joint Committee on Cancer: Cancer Staging Manual. Ophthal Plast Reconstr Surg. 2019 Feb;35(1):38-41. https://doi.org/10.1097/IOP.0000000000001133
Rogers HW, Weinstock MA, Harris AR, et al. Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Arch Dermatol. 2010 Mar;146(3):283-7. https://doi.org/10.1001/archdermatol.2010.19
Goldenberg G, Karagiannis T, Palmer JB, et al. Incidence and prevalence of basal cell carcinoma (BCC) and locally advanced BCC (LABCC) in a large commercially insured population in the United States: A retrospective cohort study. J Am Acad Dermatol. 2016 Nov;75(5):957-966.e2. https://doi.org/10.1016/j.jaad.2016.06.020
Narayanan DL, Saladi RN, Fox JL. Ultraviolet radiation and skin cancer. Int J Dermatol. 2010 Sep;49(9):978-86. https://doi.org/10.1111/j.1365-4632.2010.04474.x
Celebi ARC, Kiratli H, Soylemezoglu F. Evaluation of the 'Hedgehog' signaling pathways in squamous and basal cell carcinomas of the eyelids and conjunctiva. Oncol Lett. 2016 Jul;12(1):467-72. https://doi.org/10.3892/ol.2016.4625
Yin VT, Merritt H, Esmaeli B. Targeting EGFR and sonic hedgehog pathways for locally advanced eyelid and periocular carcinomas. World J Clin Cases. 2014 Sep 16;2(9):432-8. https://doi.org/10.12998/wjcc.v2.i9.432
Poláková K, Murárová Z. Liečba bazocelulárneho karcinómu: Štandardné postupy. MZ SR. Bratislava, 2021.
Hallaji Z, Rahimi H, Mirshams-Shahshahani M. Comparison of risk factors of single Basal cell carcinoma with multiple Basal cell carcinomas. Indian J Dermatol. 2011 Jul;56(4):398-402. https://doi.org/10.4103/0019-5154.84766
Silverman N, Shinder R. What's New in Eyelid Tumors. Asia Pac J Ophthalmol (Phila). 2017 Mar-Apr;6(2):143-152.
van Iersel CA, van de Velden HVN, Kusters CDJ, et al. Prognostic factors for a subsequent basal cell carcinoma: implications for follow-up. Br J Dermatol. 2005 Nov;153(5):1078-80. https://doi.org/10.1111/j.1365-2133.2005.06911.x
Levi F, Randimbison L, Maspoli M, et al. High incidence of second basal cell skin cancers. Int J Cancer. 2006 Sep 15;119(6):1505-7. https://doi.org/10.1002/ijc.22000
Ramachandran S, Fryer AA, Lovatt TJ, et al. Combined effects of gender, skin type and polymorphic genes on clinical phenotype: use of rate of increase in numbers of basal cell carcinomas as a model system. Cancer Lett. 2003 Jan 28;189(2):175-81. https://doi.org/10.1016/S0304-3835(02)00516-5
Karagas MR, Stukel TA, Greenberg ER, et al. Risk of subsequent basal cell carcinoma and squamous cell carcinoma of the skin among patients with prior skin cancer. Skin Cancer Prevention Study Group. JAMA. 1992 Jun 24;267(24):3305-10. https://doi.org/10.1001/jama.267.24.3305
Badri T, Zeglaoui F, Kochbati L, et al. Multiple basal cell carcinomas following radiation therapy for nasopharyngeal cancer. Presse Medicale Paris Fr 1983. 2006 Jan;35(1 Pt 1):55-7. https://doi.org/10.1016/S0755-4982(06)74520-1
Marcil I, Stern RS. Risk of developing a subsequent nonmelanoma skin cancer in patients with a history of nonmelanoma skin cancer: a critical review of the literature and meta-analysis. Arch Dermatol. 2000 Dec;136(12):1524-30. https://doi.org/10.1001/archderm.136.12.1524
Chen J, Ruczinski I, Jorgensen TJ, et al. Nonmelanoma skin cancer and risk for subsequent malignancy. J Natl Cancer Inst. 2008 Sep 3;100(17):1215-22. https://doi.org/10.1093/jnci/djn260
Revenga F, Paricio JF, Vázquez MM, Del Villar V. Risk of subsequent non-melanoma skin cancer in a cohort of patients with primary basal cell carcinoma. J Eur Acad Dermatol Venereol JEADV. 2004 Jul;18(4):514-5. https://doi.org/10.1111/j.1468-3083.2004.00956.x
Collins GL, Nickoonahand N, Morgan MB. Changing demographics and pathology of nonmelanoma skin cancer in the last 30 years. Semin Cutan Med Surg. 2004 Mar;23(1):80-3. https://doi.org/10.1016/S1085-5629(03)00089-0
Lear JT, Smith AG, Strange RC, Fryer AA. Patients with truncal basal cell carcinoma represent a high-risk group. Arch Dermatol. 1998 Mar;134(3):373. https://doi.org/10.1001/archderm.134.3.373
Lovatt TJ, Lear JT, Bastrilles J, et al. Associations between ultraviolet radiation, basal cell carcinoma site and histology, host characteristics, and rate of development of further tumors. J Am Acad Dermatol. 2005 Mar;52(3 Pt 1):468-73. https://doi.org/10.1016/j.jaad.2004.08.060
Ramachandran S, Fryer AA, Smith A, et al. Cutaneous basal cell carcinomas: distinct host factors are associated with the development of tumors on the trunk and on the head and neck. Cancer. 2001 Jul 15;92(2):354-8. https://doi.org/10.1002/1097-0142(20010715)92:2<354::AID-CNCR1330>3.0.CO;2-F
Wallberg P, Kaaman T, Lindberg M. Multiple basal cell carcinoma. A clinical evaluation of risk factors. Acta Derm Venereol. 1998 Mar;78(2):127-9. https://doi.org/10.1080/000155598433467
Wei Q, Matanoski GM, Farmer ER, et al. DNA repair related to multiple skin cancers and drug use. Cancer Res. 1994 Jan 15;54(2):437-40.
Hajeer AH, Lear JT, Ollier WE, et al. Preliminary evidence of an association of tumour necrosis factor microsatellites with increased risk of multiple basal cell carcinomas. Br J Dermatol. 2000 Mar;142(3):441-5. https://doi.org/10.1046/j.1365-2133.2000.03353.x
Strange RC, El-Genidy N, Ramachandran S, et al. PTCH polymorphism is associated with the rate of increase in basal cell carcinoma numbers during follow-up: preliminary data on the influence of an exon 12-exon 23 haplotype. Environ Mol Mutagen. 2004;44(5):469-76. https://doi.org/10.1002/em.20068
Ramachandran S, Fryer AA, Smith AG, et al. Basal cell carcinomas: association of allelic variants with a high-risk subgroup of patients with the multiple presentation phenotype. Pharmacogenetics. 2001 Apr;11(3):247-54. https://doi.org/10.1097/00008571-200104000-00008
Basset-Seguin N, Herms F. Update in the Management of Basal Cell Carcinoma. Acta Derm Venereol. 2020 Jun 3;100(11). https://doi.org/10.2340/00015555-3495
Lim LT, Agarwal PK, Young D, et al. The Effect of Socio-Economic Status on Severity of Periocular Basal Cell Carcinoma at Presentation. Ophthal Plast Reconstr Surg. 2015 Dec;31(6):456-8. https://doi.org/10.1097/IOP.0000000000000386
Furdová A, Horkovičová K, Babál P, et al. Non-melanotic Tumors of the Eyelids Skin and Inner Corner - Basocellular Carcinoma. Cesk Slov Oftalmol. 2015 Winter;71(6):293-301.
Ho SF, Brown L, Bamford M, et al. 5 Years review of periocular basal cell carcinoma and proposed follow-up protocol. Eye. 2013 Jan;27(1):78-83. https://doi.org/10.1038/eye.2012.230
Tzoutzos K, Batistatou A, Kitsos G, et al. Retrospective clinicopathological study of 129 cancerous and 18 precancerous lesions of the eyelids in North-Western Greece. Int Ophthalmol. 2017 Feb;37(1):203-8. https://doi.org/10.1007/s10792-016-0258-8
Holmes J, von Braunmühl T, Berking C, et al. Optical coherence tomography of basal cell carcinoma: influence of location, subtype, observer variability and image quality on diagnostic performance. Br J Dermatol. 2018;178(5):1102-10. https://doi.org/10.1111/bjd.16154
Bălăşoiu AT, Mănescu MR, Bălăşoiu M, et al. Histological and immunohistochemical study of the eyelid basal cell carcinomas. Romanian J Morphol Embryol Rev Roum Morphol Embryol. 2015;56(2 Suppl):803-10.
Zhang L, Huang X, Zhu X, et al. Differential senescence capacities in meibomian gland carcinoma and basal cell carcinoma. Int J Cancer. 2016 Mar 15;138(6):1442-52. https://doi.org/10.1002/ijc.29882
Quazi SJ, Aslam N, Saleem H et al. Surgical Margin of Excision in Basal Cell Carcinoma: A Systematic Review of Literature. 2020;12(7):e9211. https://doi.org/10.7759/cureus.9211
Malhotra R, Huilgol SC, Huynh NT, Selva D. The Australian Mohs database, part I: periocular basal cell carcinoma experience over 7 years. Ophthalmology. 2004 Apr;111(4):624-30. https://doi.org/10.1016/j.ophtha.2003.12.003
Malhotra R, Huilgol SC, Huynh NT, Selva D. The Australian Mohs database, part II: periocular basal cell carcinoma outcome at 5-year follow-up. Ophthalmology. 2004 Apr;111(4):631-6. https://doi.org/10.1016/j.ophtha.2003.11.004
Newlands C, Currie R, Memon A, et al. Non-melanoma skin cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol. 2016 May;130(S2):S125-32. https://doi.org/10.1017/S0022215116000554
Shi Y, Jia R, Fan X. Ocular basal cell carcinoma: a brief literature review of clinical diagnosis and treatment. OncoTargets Ther. 2017 May 8;10:2483-9. https://doi.org/10.2147/OTT.S130371
Koyfman SA, Cooper JS, Beitler JJ, et al. ACR Appropriateness Criteria(®) Aggressive Nonmelanomatous Skin Cancer of the Head and Neck. Head Neck. 2016 Feb;38(2):175-82. https://doi.org/10.1002/hed.24171
Avril MF, Auperin A, Margulis A, Gerbaulet A, Duvillard P, Benhamou E, et al. Basal cell carcinoma of the face: surgery or radiotherapy? Results of a randomized study. Br J Cancer. 1997;76(1):100-6. https://doi.org/10.1038/bjc.1997.343
Yu S-S, Zhao Y, Zhao H, Lin J-Y, Tang X. A retrospective study of 2228 cases with eyelid tumors. Int J Ophthalmol. 2018 Nov 18;11(11):1835-41.
Dirix L, Rutten A. Vismodegib: a promising drug in the treatment of basal cell carcinomas. Future Oncol Lond Engl. 2012 Aug;8(8):915-28. https://doi.org/10.2217/fon.12.82
Sekulic A, Migden MR, Basset-Seguin N, et al. Long-term safety and efficacy of vismodegib in patients with advanced basal cell carcinoma: final update of the pivotal ERIVANCE BCC study. BMC Cancer. 2017 16;17(1):332. https://doi.org/10.1186/s12885-017-3286-5
Macha MA, Batra SK, Ganti AK. Profile of vismodegib and its potential in the treatment of advanced basal cell carcinoma. Cancer Manag Res. 2013;5:197-203. https://doi.org/10.2147/CMAR.S45976
Yin VT, Pfeiffer ML, Esmaeli B. Targeted therapy for orbital and periocular basal cell carcinoma and squamous cell carcinoma. Ophthal Plast Reconstr Surg. 2013 Apr;29(2):87-92. https://doi.org/10.1097/IOP.0b013e3182831bf3
Erdem GU, Sendur MAN, Ozdemir NY, et al. A comprehensive review of the role of the hedgehog pathway and vismodegib in the management of basal cell carcinoma. Curr Med Res Opin. 2015 Apr;31(4):743-56. https://doi.org/10.1185/03007995.2015.1018988
Gill HS, Moscato EE, Chang ALS, et al. Vismodegib for periocular and orbital basal cell carcinoma. JAMA Ophthalmol. 2013 Dec;131(12):1591-4. https://doi.org/10.1001/jamaophthalmol.2013.5018
Papastefanou VP, René C. Secondary Resistance to Vismodegib After Initial Successful Treatment of Extensive Recurrent Periocular Basal Cell Carcinoma with Orbital Invasion. Ophthal Plast Reconstr Surg. 2017 Jun;33(3S Suppl 1):S68-70. https://doi.org/10.1097/IOP.0000000000000565
Sekulic A, Migden MR, Lewis K et al. ERIVANCE BCC investigators. Pivotal ERIVANCE basal cell carcinoma (BCC) study: 12-month update of efficacy and safety of vismodegib in advanced BCC. J Am Acad Dermatol. 2015 Jun;72(6):1021-6.e8. https://doi.org/10.1016/j.jaad.2015.03.021
Fahradyan A, Howell AC, Wolfswinkel EM, et al. Updates on the Management of Non-Melanoma Skin Cancer (NMSC). Healthc Basel Switz. 2017 Nov 1;5(4). https://doi.org/10.3390/healthcare5040082
Garcia-Martin E, Gil-Arribas LM, Idoipe M, et al. Comparison of imiquimod 5% cream versus radiotherapy as treatment for eyelid basal cell carcinoma. Br J Ophthalmol. 2011 Oct;95(10):1393-6. https://doi.org/10.1136/bjo.2010.193078
Coker DD, Elias EG, Viravathana T et al. Chemotherapy for Metastatic Basal Cell Carcinoma. Arch Dermatol. 1983; 119(1):44-50. https://doi.org/10.1001/archderm.1983.01650250048015
Cisek P, Kieszko D, Bilski M. Interstitial HDR Brachytherapy in the Treatment of Non-Melanocytic Skin Cancers around the Eye. Cancers, 13(6),1425. https://doi.org/10.3390/cancers13061425
Velter C. Place de la radiothérapie dans le traitement du carcinome basocellulaire. Ann Dermatol Vénéréologie. 2018 Nov 1;145:VS30-5. https://doi.org/10.1016/S0151-9638(18)31256-0
Leibowitch I, McNab A, Sullivan T, et al. Orbital Invasion by Periocular Basal Cell Carcinoma. Ophtalmology, 2005; 112: 717-723. https://doi.org/10.1016/j.ophtha.2004.11.036
Honavar SG, Manjandavida FP. Tumors of the ocular surface: A review. Indian J Ophthalmol. 2015 Mar;63(3):187-203. https://doi.org/10.4103/0301-4738.156912
Süngü N, Kiran MM, Tatli Doğan H, el al. Evaluation of p53 and Ki67 Expression Profiles in Basal Cell Carcinomas in a Usual and an Unusual Location. Turk Patoloji Derg. 2018;34(2):165-70. https://doi.org/10.5146/tjpath.2018.01424
Kramer E, Herman O, Frand J, et al. Ki67 as a biologic marker of basal cell carcinoma: a retrospective study. Isr Med Assoc J IMAJ. 2014 Apr;16(4):229-32.
Staibao S, Lo Muzio L, Pannone G. Interaction between bcl-2 and P53 in neoplastic progression of basal cell carcinoma of the head and neck. Anticancer Res. 2001 Nov-Dec;21(6A):3757-64.
##submission.downloads##
Опубліковано
Як цитувати
Номер
Розділ
Ліцензія
Авторське право (c) 2023 Prídavková Z., Furdová A., Benca Kapitánová K., Vida R., Žiak P., Popov I.

Ця робота ліцензується відповідно до Creative Commons Attribution 4.0 International License.
Ця робота ліцензується відповідно до ліцензії Creative Commons Attribution 4.0 International (CC BY). Ця ліцензія дозволяє повторно використовувати, поширювати, переробляти, адаптувати та будувати на основі матеріалу на будь-якому носії або в будь-якому форматі за умови обов'язкового посилання на авторів робіт і первинну публікацію у цьому журналі. Ліцензія дозволяє комерційне використання.
ПОЛОЖЕННЯ ПРО АВТОРСЬКІ ПРАВА
Автори, які подають матеріали до цього журналу, погоджуються з наступними положеннями:
- Автори отримують право на авторство своєї роботи одразу після її публікації та назавжди зберігають це право за собою без жодних обмежень.
- Дата початку дії авторського права на статтю відповідає даті публікації випуску, до якого вона включена.
ПОЛІТИКА ДЕПОНУВАННЯ
- Редакція журналу заохочує розміщення авторами рукопису статті в мережі Інтернет (наприклад, у сховищах установ або на особистих веб-сайтах), оскільки це сприяє виникненню продуктивної наукової дискусії та позитивно позначається на оперативності і динаміці цитування.
- Автори мають право укладати самостійні додаткові угоди щодо неексклюзивного розповсюдження статті у тому вигляді, в якому вона була опублікована цим журналом за умови збереження посилання на первинну публікацію у цьому журналі.
- Дозволяється самоархівування постпринтів (версій рукописів, схвалених до друку в процесі рецензування) під час їх редакційного опрацювання або опублікованих видавцем PDF-версій.
- Самоархівування препринтів (версій рукописів до рецензування) не дозволяється.